Research Article: Journal of Drug and Alcohol Research (2023) Volume 12, Issue 9
Lead-Induced Hepatotoxicity: Mechanisms and Therapy
C.H. Hari Kumar1, Mounika Vinusha Regidi2 and Swathi Putta2*2Department of Pharmacy, Raghu College of Pharmacy, India
Swathi Putta, Department of Pharmacy, Raghu College of Pharmacy, India, Email: swathidbmp@gmail.com
Received: 02-Oct-2023, Manuscript No. JDAR-23-111352; Editor assigned: 04-Oct-2023, Pre QC No. JDAR-23-111352 (PQ); Reviewed: 18-Oct-2023, QC No. JDAR-23-111352; Revised: 23-Oct-2023, Manuscript No. JDAR-23-111352 (R); Published: 30-Oct-2023, DOI: 10.4303/JDAR/236262
Abstract
Lead is a dangerous substance that can cause harm to those who are exposed to it at work. The negative effects of lead exposure are well-documented and can lead to serious health issues. In fact, high levels of lead can increase the risk of liver damage by three times. In this comprehensive review, we discuss various sources of lead, types of lead poisoning, safe doses and toxicity levels of lead exposure, and the mechanism of lead-induced liverdamage. We also cover available therapies for lead poisoning and explore the potential of herbal remedies in treating lead-induced liver damage.
Keywords
Lead; Hepatotoxicity; Herbal remedies
Introduction
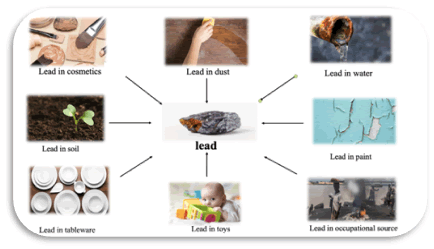
Lead is a heavy metal that is present in the environment in various forms, including metallic lead and its organic and inorganic salts. It has been used since ancient times, particularly by the Romans, who used it for various industrial applications such as manufacturing tableware, water pipes, and other daily-use items. Lead compounds were also used as medicines for both internal and external applications [1]. For instance, the “sugar of lead” was used as a sweetening agent and a possible antibacterial agent in wine production until the 19th century. However, in the 20th century, it became evident that lead is a highly toxic substance that should not be used in therapeutic applications or as food additives [2]. Its use in fuel was eliminated to reduce lead emissions, and emission from metal smelting and ore processing plants was restrained [3]. Despite the ban on lead in many countries, it is still used in various industries due to its valuable characteristics like malleability, softness, poor conductibility, resistance to corrosion, and ductility. However, the continuous use of lead has led to environmental accumulations and hazards due to its non-biodegradable nature [4] (Figure 1).
Sources of lead exposure
Lead in paint: Before 1978, lead was commonly used in household paint. However, the Consumer Product Safety Commission restricted its use in order to prevent lead poisoning. Unfortunately, many buildings constructed before this time still contain lead-based paint, with approximately 74% of its remaining. Houses built prior to 1950 are particularly concerning, as they are more likely to have used lead-based paint [5]. Children are at a higher risk of exposure to lead paint through direct and indirect means, especially if they live in older homes with deferred maintenance. Lead dust from the paint can be ingested and is hazardous. Old toys, furniture, and playground equipment that were painted with lead-based paint also have high levels of lead content.
Figure 1: Sources of lead toxicity
Lead in dust: Children are often exposed to lead paint dust, which is easily absorbed and a common source of contamination. Damaged painted walls can contaminate the interior of a house with lead or lead dust, and when painted surfaces rub against each other, fine lead dust is formed and contaminates the air. This dust can accumulate on carpets, toys, and other objects, especially on floors, where children are at risk of ingesting it by putting their contaminated hands in their mouths. A study has shown that the amount of lead in house paint has a greater association with Blood Lead Levels (BLLs) in young children than the quantity of lead dust in the house [6]. Additionally, statistical analysis of 12 new studies has shown a connection between lead in the dust and BLLs among children aged 6 months-36 months, with a linear relationship between lead dust accumulation and the risk of elevated BLLs [7].
Lead exposure
Acute exposure: When someone is experiencing acute poisoning, they may experience neurological symptoms such as pain, weakened muscle strength, sensory abnormalities, and sometimes even brain inflammation. Additionally, there may be digestive-related symptoms like stomach pain, nausea, vomiting, diarrhea, and constipation [8]. If a person ingests a large amount of lead in a short period of time, it can cause shock due to water loss in the digestive system, and haemolytic action can occur, which may result in symptoms like anemia and haematuria. When kidney damage occurs, urine output decreases. People with acute lead exposure may also display similar symptoms to those with chronic lead exposure [9].
Chronic exposure: If someone is exposed to lead over a long time, they may experience various symptoms related to their digestive, nervous, and neurological systems. These symptoms can be different depending on the duration and strength of the exposure. For instance, neurological symptoms may appear if the exposure is strong but short, while digestive system symptoms may arise from long-term exposure. Some symptoms of chronic lead exposure include anemia, fatigue, reduced limb sensation, stomachache, nausea, vomiting, depression, and reduced concentration and memory, according to a study by L. Patrick et al., [10]. Chronic lead poisoning may also result in a grey tint to the skin or a blue line in the gums, known as the Burton line, as stated by R. Josef et al., [11]. Moreover, chronic lead exposure may lead to optic neuritis-induced scotoma and vision impairments.
Lead exposure in pregnancy and children: It has been found that exposure of a developing embryo or fetus to lead while in the womb can increase the likelihood of premature birth and low birth weight [12]. Due to their smaller body size and faster absorption of lead, children are more susceptible to lead poisoning. Additionally, as babies crawl on the floor and put various objects in their mouths, they are more likely to come into contact with lead. Symptoms commonly seen in children include loss of appetite, stomach pain, vomiting, learning difficulties, behavioral issues, and anemia. In cases of high levels of lead exposure, symptoms of leukonychia striata may be observed [13].
Adverse effects: At levels above 80 μg/dL, serious, permanent health damage may occur (extremely dangerous).
• Between 40 μg/dL and 80 μg/dL, serious health damage may be occuring, even if there are no symptoms (seriously elevated).
• Between 25 μg/dL and 40 μg/dL, regular exposure is occuring. There is some evidence of potential physiologic problems (elevated).
• Between 10 μg/dL and 25 μg/dL, lead is building up in the body and some exposure is occurring typical level for U.S. adults is less than 10 μg/dL.
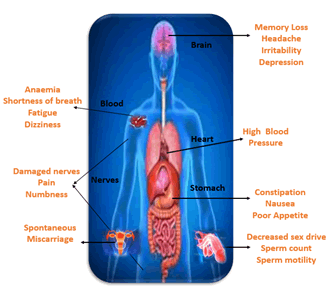
Dose/toxicity: It is rare for lead poisoning to occur, as the lethal dose of most lead salts is 10 g/70 kg, while it is 100 mg for tetra ethyl leads. However, lead can harm all systems in the body and impede enzymes necessary for cell function. It can alter the structure and function of the kidneys, bones, central nervous system, and hematopoietic system, and cause biochemical, histopathological, neuropsychological, teratogenic, and reproductive effects. The symptoms of lead poisoning are dependent on the dose, with life-threatening encephalopathy occurring in children at blood lead levels of 70 mg/dl. These symptoms may include lethargy, abdominal cramps, anorexia, irritability, vomiting, clumsiness, ataxia, hyper irritability, stupor, coma, and seizures. Neurological signs and mental retardation may also occur (Figure 2).
Figure 2: Symptoms of lead toxicity
However, due to the prohibition of leaded paint in 1978 and the elimination of leaded gasoline in 1985, cases of children with lethal blood lead levels are now rare in the United States. Those who do present with poisoning symptoms may complain of stomach pains and loss of appetite or even have anemia. However, these symptoms do not always point to lead exposure. Low levels of lead may still have neurotoxic effects, affecting neuro-behavioral functioning.
The Occupational Safety and Health Act (OSHA) were passed in 1971, with a Permissible Exposure Level (PEL) of 200 mg/ml for lead dust in the air. In 1979, a permanent OSHA standard was implemented, with a PEL of 40 mg/ ml and a blood lead concentration limit of 50 μg/dl. The Centers for Disease Control defines an elevated BLL as 10 Ag/dL, which has been continually reduced over the past few decades. Studies have shown that adverse health effects can occur at BLLs below 10 Ag/dL, and there is no identified threshold for harmful effects of postnatal lead exposure. Low-leaded gasoline (0.15g/L) was made available in major cities in India in 1994 and was later expanded to the entire country in 1996.
Lead poisoning is 2 types i.e.,
Acute poisoning: Acute poisoning is a rare occurrence, and many reported cases of acute poisoning may actually be caused by a sudden release of significant amounts of lead into the bloodstream from bone, exacerbating chronic lead poisoning. Symptoms of acute poisoning may include a metallic taste, abdominal pain, constipation or diarrhea (with blackish stools due to lead sulphide), vomiting, hyperactivity or lethargy, ataxia, behavioral changes, convulsions, and coma.
Chronic poisoning (plumbism or saturnism): On the other hand, chronic poisoning, also known as plumbism or saturnism, may present differently in children and adults. Children may experience weight loss, weakness, and anemia, and their first signs of poisoning may be subtle neurobehavioral deficits that adversely affect their classroom behavior and social interaction. Adults may manifest vague gastrointestinal and CNS complaints, and wrist drop and colic are rare occurrences.
For women of child-bearing age and young individuals under 18, there are lower action and suspension levels in place. If a woman is pregnant, the lead in her blood can transfer to the blood of her developing baby, which can potentially affect its growth. Therefore, it’s crucial to keep lead levels in one’s blood as low as possible during pregnancy. Once a woman becomes pregnant, the doctor will automatically recommend avoiding work that involves significant exposure to lead. It’s highly recommended to inform your employer as soon as possible after confirming the pregnancy for the benefit of the baby’s well-being (Table 1). The law also provides greater protection to young people under 18 since they usually have less experience working with hazardous substances like lead. It is strictly prohibited for women capable of having children and young individuals under 18 to work in lead smelting, refining, and most jobs in the manufacture of lead-acid batteries (Table 2).
Table 1: Levels of lead toxicity according to severity
| Mild Toxicity (BL 40 to 60 mcg/100 mL) | Moderate Toxicity (BL 60 to 100 mcg/100 mL) | Severe toxicity (BL more than 100 mcg/100 mL) |
|---|---|---|
| Myalgia Paraesthesia Fatigue Irritability Abdominal discomfort | Arthralgia (Especially nocturnal) Muscular exhaustibility Tremor, Headache Diffuse abdominal pain Anorexia, metallic taste, Vomiting, Constipation Weight loss, Hypertension | Lead palsy-Wrist or foot drop A bluish black lead line on gums (Barton’s line)
|
Table 2: Lead levels in each age category
| Category | Action level | Suspension level |
|---|---|---|
| General employees | 50 g/dl | 60 µg/dl |
| Women of child-bearing age | 30 µg/dl | 30 µg/dl |
| Young people under 18 other than at (a) | 40 µg/dl | 50 µg/dl |
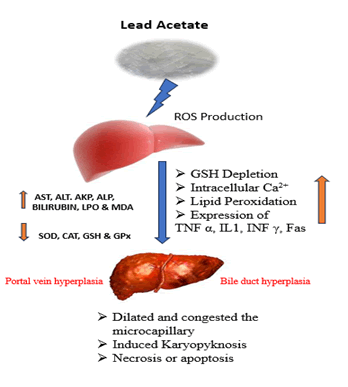
Effect on lead on liver: Studies have been conducted to evaluate the effects of lead exposure on liver function. However, most of the available research has compared the hepatic effects in workers with PbB levels greater than 10 μg/dL to those with lower levels. The results of these studies have been inconsistent and do not show any clear exposure-response relationships. Liver enlargement and thickening of the gallbladder wall have been observed in workers with mean PbB levels of at least 28.66 μg/ dL, which indicates oxidative stress. However, the histopathological effects of lead on the liver have not yet been established. Some studies have suggested that PbB levels greater than 10 μg/dL may lead to elevated plasma liver enzymes and total cholesterol levels, as well as an enlarged liver and thicker gallbladder wall (Figure 3).
Lead toxicity primarily affects heme synthesis enzymes, thiol-containing antioxidants and enzymes (such as superoxide dismutase, catalase, glutathione peroxidase, glucose 6-phosphate dehydrogenase), and antioxidant molecules like GSH. Even low levels of lead in the blood can inhibit the activity of these enzymes, resulting in the generation of reactive oxygen species and exacerbating oxidative stress. This stress plays an important role in the pathogenesis of lead-induced toxicity and related diseases. The central nervous system is the primary target of lead toxicity, and it can cause cellular, intracellular, and molecular mechanisms such as induction of oxidative stress, neurocites apoptosis intensification, and interfering with Ca (2+)-dependent enzymes like nitric oxide synthase [14].
Figure 3: Mechanism of lead-induced hepatotoxicity
Preventions to decrease lead toxicity: To protect your child from lead poisoning, it’s important to identify and address any lead in your home. This is especially common in homes built before 1978, where lead paint may still be present. It’s recommended to have a licensed lead inspector inspect your home before any remodelling or renovation work is done. Old paint that cracks and peels can create lead dust, which is harmful to children if ingested through their hands or toys. To clean up lead dust, use wet paper towels and clean around windows, play areas, and floors. Wash hands and toys frequently with soap and water, especially before eating and sleeping. You can also cover chipping or peeling paint with contact paper or duct tape. Give your child healthy foods.
Feed your child healthy foods with calcium, iron, and vitamin C
These foods may help keep lead out of the body.
• Calcium is in milk, yogurt, cheese, and green leafy vegetables like spinach.
• Iron is in lean red meats, beans, peanut butter, and cereals.
• Vitamin C is in oranges, green and red peppers, and juice.
If you work with home repairs that involve sanding or scraping paint, be sure to change your clothing and shoes and shower when you get home to avoid exposing your family to lead. Pregnant individuals should also be cautious, as lead poisoning can harm a fetus even before birth. High levels of lead in the blood can increase the risk of miscarriage, premature birth, brain and nervous system damage, kidney damage, and learning or behavioral problems in children.
Drugs available for lead intoxication
Some common chelating agents used against lead poisoning are given below:
1. Calcium Disodium Ethylene Diamine Tetraacetic Acid (CaNa2 EDTA)
2. D-penicillamine
3. Meso 2,3-Dimercaptosuccinic Acid (DMSA)
4. Sodium 2,3-Dimercaptopropane-1-Sulphonate (DMPS).
Chelation therapy: In this treatment, a medication given by mouth binds with the lead so that it’s excreted in the urine. Chelation therapy might be recommended for children with a blood level of 45 mcg/dl of lead.
EDTA chelation therapy: Healthcare providers treat adults with lead levels greater than 45 mcg/dl of blood and children who can’t tolerate the drug used in conventional chelation therapy most commonly with a chemical called Calcium Disodium Ethylenediaminetetraacetic Acid (EDTA). It is given by injection.
Trade names are: Fairgenol-H
Succimer: Succimer is a lead chelator, prescribed for the treatment of lead poison.
Herbal drug therapy: There has been a growing focus on the use of herbal medicines in recent times. Many plantbased products are known to contain antioxidants that can help prevent oxidative stress. Synthetic antioxidants have been found to have side effects, so there is a growing interest in using plant extracts instead. Studies have shown that crude extracts of many plants can help alleviate the toxic effects of lead. This is mainly due to the flavonoids present in these plants, which have antioxidant properties. Antioxidants are now widely recognized to play a crucial role in treating lead poisoning in humans, as lead toxicity can affect various organs, such as the brain, kidneys, and liver.
Cayratia carnosa: Lead acetate-20 mg/Kg/b.wt/i.p for 1 day
The effectiveness of methanol extract in protecting the liver was examined in rats with lead acetate-induced liver damage. The study measured changes in biochemical markers of liver damage such as ALT, AST, ALP, ACP, and LDH, as well as serum parameters including cholesterol, triglycerides, and bilirubin levels in both the lead acetatetreated and untreated groups. The group exposed to lead acetate showed increased levels of ALT, AST, ALP, ACP, and LDH, as well as elevated serum parameters in the liver such as cholesterol, triglycerides, and bilirubin. However, treatment with methanolic extract from the leaves of Cayratia carnosa (at a dose of 250 mg/kg/bwt) resulted in a dose-dependent reduction of the elevated levels of biochemical markers, bringing them back to near-normal levels [15].
Tinospora cordifolia: Lead nitrate-5 mg/kg/B.W/oral for 30 days
Mice treated with lead showed low levels of tissue enzymes such as SOD and CAT, and high levels of enzymes like AST, ALT, ALP, and ACP. However, when given an oral dose of aqueous stem extract (400 mg/kg body weight) and aqueous leaves extract (400 mg/kg body weight) along with lead nitrate (5 mg/kg body weight, i.p. for 30 days), their SOD and CAT activities increased, while their AST, ALT, ALP, and ACP enzyme levels decreased. Histopathology/ histological examinations of liver sections confirmed these biochemical observations. This study demonstrated that the plant extracts can protect against lead-induced hepatic damage [16].
Asparagus racemosus: Lead nitrate-20 mg/Kg body weight/oral for 45 days
The study examined the effects of lead nitrate and ARRE, both independently and in combination, on the liver. Results showed that ARRE had a significant hepatoprotective effect on mice exposed to lead, compared to the control group. Lead nitrate administration caused a decrease in the levels of SOD, CAT, and reduced GSH while increasing the level of lipid peroxidation. On the other hand, ARRE administration significantly improved all of these parameters. The lead-treated group had decreased levels of AST, ALT, ALP, and bilirubin, while the ARRE-treated groups had significant increases in these levels. Additionally, the total protein and albumin levels were significantly increased in the ARRE-treated groups, while decreased in the lead-treated group [17].
Leucas aspera: Lead acetate-50 mg/kg/b.wt/oral for 21 days
The effect of a 400 mg/kg dose of hydroalcoholic leaf extract of Leucas aspera on male albino Wistar rats was studied during exposure to an oral dose of 50 mg/kg of lead acetate. 6 rats were used in each group and their liver function was evaluated. The results showed that the dose of 400 mg/kg of hydroalcoholic leaf extract of Leucas aspera significantly reduced liver enzymes in a dose-dependent manner (P<0.05) [18].
Zingiber officinale Roscoe: Lead acetate-500 ppm by oral 50 for days
Researchers investigated how a ginger solution affected liver damage caused by lead-induced oxidative stress in rats. The rats were given lead acetate in their drinking water for 50 days, resulting in liver damage shown by increased levels of ALT, AST, and ALP, depleted hepatic GSH, elevated MDA concentration, and decreased GPx. However, when the rats were treated with whole ginger, these parameters improved, indicating ginger’s potential to alleviate lead-induced liver damage caused by oxidative stress in rats [19].
Spirulina: Lead acetate-1.89 mg/kg for 7 days
The effects of lead acetate on the liver and kidney tissues of male albino wister rats were examined through light microscopy. The rats were exposed to a sublethal concentration of 1.896 mg/kg body weight of lead acetate for 7 days, with a control group left untreated. Two other groups were given spirulina at a dosage of 2 mg/kg body weight along with the lead acetate. The liver and kidney tissues were then studied histologically. No pathological changes were observed in the untreated control and spirulina alone groups. The lead acetate treated group experienced severe histological changes, while the group treated with both lead acetate and spirulina showed signs of cell recovery [20].
Coriandrum sativum: Lead nitrate-40 mg/kg/b.wt/oral for 7 days
The study examined the impact of lead on liver and kidney oxidative stress, biochemical changes, and soft tissue histopathology. The results revealed that lead nitrate treatment increased LPO levels in the liver and kidney, but this effect was reduced by plant extracts. Additionally, lead caused a decrease in antioxidant enzyme activity, which was reversed by treatment with plant extract. Coriander extract was particularly effective in mitigating the negative effects of lead on biochemical parameters related to hepatic and renal oxidative stress. Oral administration of Coriander to lead-treated mice also partially reversed histopathological changes. In conclusion, Coriandrum sativum can protect against lead toxicity, as evidenced by these findings [21].
Ocimum sanctum linn: Lead acetate-2.10 mg/150 g/b.wt/ oral for 3 days
Lead was used to cause hepatotoxicity in animals. The plant drug was orally administered to the animals for 21 days. The levels of AST, ALT, ALP, GGT, Serum Protein, Serum Bilirubin, and Tissue Glycogen in the liver were analyzed, as well as the activity of GSH and SOD to assess the antioxidant status. The extent of Lipid Peroxidation (LPO) was also measured. The results showed that the selected drug source has a protective effect. The liver injury caused by lead resulted in a significant increase in serum marker enzyme levels, along with an increase in serum bilirubin content. The liver was found to be inactive due to the decreased levels of serum protein and tissue glycogen levels. The antioxidant status was also low, causing an accumulation of lipid peroxides in the hepatic tissues. However, treatment with the aqueous extract of O.sanctum restored all studied parameters to near-normal levels, as shown in a study by N. Akilavalli et al., (2011) [22].
Vitis vinifera: Lead acetate-100 mg/kg/b.wt/ip-7 days
This study aimed to investigate the protective and therapeutic effects of GSE on lead-induced neuro and hepato-toxicity in rats. The study evaluated the levels of Norepinephrine (NE), Dopamine (DA), serotonin (5-HT), and 5-hydroxyindol acetic acid (5-HIAA) in different brain regions, including the cerebellum, brainstem, striatum, cerebral cortex, hypothalamus, and hippocampus. Results showed that the subacute dose of LA (100 mg/kg/day, i.p.) significantly decreased NE, DA, 5-HT, and 5-HIAA content in all tested brain regions. Moreover, the data revealed a significant increase in liver enzymes, including SGOT, SGPT, and LDH levels [23].
Turmeric and myrrh: Lead acetate-0.5% oral-8 weeks El- I.M. Ashmawy et al., (2006). The study involved adding lead acetate and varying amounts of turmeric and myrrh powder to a standard diet. The results showed a decrease in GSH levels and an increase in MDA levels with the addition of lead. However, adding the protective plants resulted in a significant reversal of these effects. The study also confirmed the genotoxicity of lead through a reduction in dividing cells, an increase in aberrant cells, and an increase in chromosomal aberrations. Treatment with the protective plants reduced the genotoxicity caused by lead, with the strongest protection observed with 5% turmeric powder [24].
Curcuma longa: Lead acetate-1000 mg/kg/b.wt/oral for 28 days
After being given lead acetate orally for 28 days, AST, ALT), and ALP levels increased significantly. Additionally, there was a significant increase in Lipid Peroxidation (LPO) and a decrease in SOD and GSH levels, while lead accumulation in the liver increased. However, administering Curcuma longa at 500 mg/kg BW significantly reduced elevated ALP, AST, ALT, and LPO levels (P<0.01), and increased GSH levels (p<0.05) compared to the lead acetate treated group. There was no significant difference in SOD level and lead concentration in the liver compared to the lead acetate-treated group [25].
Green tea: Lead acetate-0.4% oral for 8 weeks
A study showed that lead exposure can reduce the liver’s ability to fight against harmful substances, but this effect can be reversed by taking green tea extract. The levels of liver enzymes and serum protein also indicated that green tea extract has protective properties. Histopathological analysis of the liver showed that green tea extract caused mild degeneration and congestion of blood vessels, but it also enhanced the liver’s ability to regenerate [26].
Salidroside: Lead acetate solution of 500 ppm for 60 days
Exposure to lead has been found to cause a significant increase in the levels of serum ALP, AST, ALT, and TB (P<0.01). However, treatment with salidroside for 60 days has been shown to reverse these effects. Additionally, lead acetate exposure has been found to significantly decrease liver GSH, SOD, and GSH-Px levels, MDA levels were also found to be significantly increased in the PbAc group, but significantly decreased in the SDS treatment group. SDS has also been found to improve lead-induced congestion and necrosis of hepatocytes. Treatment with SDS significantly reversed the expressions of CYP2E1 and NOX2 in the liver of lead-exposed rats [27].
Curcumin: Lead acetate 50 mg/kg (i.p.) for seven consecutive days.
Liver injury caused by Pb(II) can be detected through elevated levels of ALT, AST, and LDH, as well as histopathological changes such as hepatocyte degeneration and increased collagen deposition. The CUR and/or AA have been found to improve liver function and prevent tissue injury by reducing oxidative stress, DNA damage, NF-κB, JNK, and caspase-3. CUR and/or AA also activate Akt and inhibit GSK-3β in Pb(II)-induced rats. In conclusion, CUR can prevent Pb(II) hepatotoxicity by reducing oxidative injury and inflammation and activating Akt while inhibiting GSK-3β [28].
Zingerone: A study was conducted on the protective effects of zingerone against lead-induced toxicity in Wistar rats. The concentration of ALAD in the kidney and liver tissues increased with zingerone treatment, indicating its effectiveness. Zingerone was found to improve kidney and liver histology, as well as antioxidant enzyme activity such as CAT, SOD, GPx, and GR. It also showed improvement in organ function parameters, lipid profile, and reduced levels of LPO. Thus, zingerone pretreatment holds promise as a potential agent to alleviate oxidative damage caused by lead in cells [29].
Conclusion
It is widely known that lead has no purpose in the human body and can cause severe and irreversible health issues upon entry. It can negatively impact vital organ systems such as the nervous, renal, cardiovascular, and hematopoietic systems. The generation of ROS as a result of lead exposure can lead to critical damage to biomolecules such as proteins, enzymes, DNA, and membrane-based lipids. Moreover, it can impair the body’s antioxidant defense system. Chelation therapy is currently the primary treatment for lead toxicity, which involves removing lead from the body’s various sites and expelling it through urine. To avoid lead-induced toxicity and oxidative stress, prevention is the best approach, which involves the inclusion of numerous natural and synthetic antioxidants. Several naturally occurring antioxidants such as flavonoids, vitamins, and herbal antioxidants have been found to prevent and treat lead-induced toxicity and oxidative stress.
Acknowledgement
None.
Conflict Of Interest
Authors have no conflict of interest to declare.
References
- J.O. Nriagu, Saturnine drugs and medicinal exposure to lead: A historical outline, CRC Press Boca Raton, (1992):3-22.
- J.L. Pirkle, D.J. Brody, E.W. Gunter, R.A. Kramer, D.C. Paschal, et al. The decline in blood lead levels in the United States. The National Health and Nutrition Examination Surveys (NHANES), JAMA, 272(1994):284-91.
- S. Machiej, Molecular mechanisms of lead toxicity, JBCBB, 95(2014):137-49.
- A.L. Wani, A. Ara, J.A. Usmani, Lead toxicity: A review, Intradiscal Toxicon, 8(2015):55-64.
- K.T. Ferguson, R.C. Cassells, J.W. MacAllister, G.W. Evans, The physical environment and child development: An international review, Int J Psyche, 48(2013):437-68.
- E. Gould, Childhood lead poisoning: Conservative estimates of the social and economic benefits of lead hazard control, Environ Health Perspecta, 117(2009):1162-7.
- M. Dhimal, K.B. Karki, K.K. Aryal, B. Dhimal, H.D. Joshi, et al. Correction: High blood levels of lead in children aged 6-36 months in Kathmandu Valley, Nepal: A cross-sectional study of associated factors, PLoS One, 12(2017):e0185773.
- J.M.S. Pearce, Burton's line in lead poisoning, Eur Neurol, 57(2006):118-9.
- R. Hilal-Dandan, L. Brunton, Goodman and Gilman's manual of pharmacology and therapeutics, 2013
- L. Patrick, Lead toxicity, a review of the literature. Part 1: Exposure, evaluation, and treatment, Altern Med Rev, (2006):2-22.
- R. Josef, Industrial poisoning from fumes, gases and poisons of manufacturing processes, Hard Press Pub, 2013.
- C.M. Taylor, J. Golding, A.M. Emond, Adverse effects of maternal lead levels on birth outcomes in the ALSPAC study: A prospective birth cohort study, BJOG, 122(2015):322-8.
- P.J. Landrigan, C.B. Schechter, J.M. Lipton, M.C. Fahs, J. Schwartz, Environmental pollutants and disease in American children: Estimates of morbidity,mortality, and costs for lead poisoning, asthma, cancer, and developmental disabilities, Environ Health Perspect, 110(2002):721-8.
- K. Nemsadze, T. Sanikidze, L. Ratiani, L. Gabunia, T. Sharashenidze, Mechanisms of lead-induced poisoning, Georgian Med News, 172(2009):92-6.
- V. Suganthi, S. Gowri, K. Gurusamy, Hepatoprotective activity of Cayratia carnosa on liver damage caused by lead acetate in rats, J Nat Prod Plant Resour, 3(2013):76-79.
- V. Sharma, D. Pandey, Protective role of Tinospora cordifolia against lead-induced hepatotoxicity, Toxicol Int, 17(2010):12.
- V. Sharma, R.B. Verma, S. Sharma, Preliminary evaluation of the hepatic protection by pharmacological properties of the aqueous extract of Asparagus racemosus in lead loaded Swiss albino mice, Int J Pharm Pharm Sci, 4(2012):55-62.
- M. Thenmozhi, M. Dhanalakshmi, K.M. Devi, K. Sushila, S. Thenmozhi, Evaluation of hepatoprotective activity of Leucas aspera hydroalcoholic leaf extract during exposure to lead acetate in male albino Wistar rats, Asian J Pharm Clin Res, 6(2013):78-81.
- A.M. Attia, F.A. Ibrahim, G.M. Nabil, S.W. Aziz, Antioxidant effects of ginger (Zingiber officinale Roscoe) against lead acetate-induced hepatotoxicity in rats, Afr J Pharm Pharmacol,7(2013):1213-19.
- K. Hemalatha, K. Pugazhendy, K. Jayachandran, C. Jayanthi, M. Meenambal, Studies on the protective efficacy of Spirulina against lead acetate induced hepatotoxicity in Rattus norvegicus, Int J Chem Anal Sci, 6(2012):0-15.
- L. Kansal, V. Sharma, A. Sharma, S. Lodi, S.H. Sharma, Protective role of Coriandrum sativum (coriander) extracts against lead nitrate induced oxidative stress and tissue damage in the liver and kidney in male mice, Int J Applied Biology Pharmaceutical Tech, 2(2011):65-83.
- N. Akilavalli, J. Radhika, P. Brindha, Hepatoprotective activity of Ocimum sanctum Linn. against lead-induced toxicity in albino rats, Asian J Pharmaceutical Clin Res, 4(2011):84-87.
- M. Abeer, Grape seed extract (Vitisvinifera) alleviate neurotoxicity and hepatotoxicity induced by lead acetate in male albino rats, J Behav Brain Sci, 2(2012):12-19.
- I.M. El-Ashmawy, K.M. Ashry, A.F. El-Nahas, O.M. Salama, Protection by turmeric and myrrh against liver oxidative damage and genotoxicity induced by lead acetate in mice, Basic Clin Pharmacol Toxicol, 98(2006):32-7.
- S.L. Baxla, R.H. Gora, P. Kerketta, N. Kumar, B.K. Roy, et al. Hepatoprotective effect of Curcuma longa against lead induced toxicity in wistar rats, Vet World, 6(2013):664-67.
- E.E. Mehana, A.R.M.A. Meki, K.M. Fazili, Ameliorated effects of green tea extract on lead induced liver toxicity in rats, Exp Toxicol Pathol, 64(2012):291-95.
- C. Chen, B. Lin, S. Qi, J. He, H. Zheng, Protective effects of salidroside on Lead Acetate-induced oxidative stress and hepatotoxicity in sprague-dawley rats, Biol Trace Elem Res, 191(2019):426-434.
- Alhusaini, L. Fadda, I.H. Hasan, E. Zakaria, A.M. Alenazi, et al. Curcumin ameliorates lead-induced hepatotoxicity by suppressing oxidative stress and inflammation, and modulating akt/gsk-3β signaling pathway, Biomolecules, 9(2019):703.
- Amin, I. Hussain, M.U. Rehman, B.A. Mir, S.A. Ganaie, et al. Zingerone prevents lead-induced toxicity in liver and kidney tissues by regulating the oxidative damage in wistar rats, J Food Biochem, 45(2021):e13241.
Copyright: © 2023 C.H. Hari Kumar, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.