Research Article - Journal of Drug and Alcohol Research ( 2023) Volume 0, Issue 0
Left Ventricular End Systolic Volume as an Indicator of Remodelling after Myocardial Necrosis after the Spect Examination with Technetium Tetrofosmin Drug
Hilfan AP Lubis1*, Manoefris Kasim2, Elen Sahara2 and Celly A Atmadikoesoemah12Department of Cardiology and Vascular Medicine, University of Indonesia, Jakarta, Indonesia
Hilfan AP Lubis, Department of Cardiology and Vascular Medicine, Universitas Sumatera Utara, Indonesia, Email: Hilfan.ade@usu.ac.id
Received: 02-Jan-2023, Manuscript No. JDAR-23-86260; Editor assigned: 04-Jan-2023, Pre QC No. JDAR-23-86260 (PQ); Reviewed: 18-Jan-2023, QC No. JDAR-23-86260; Revised: 23-Jan-2023, Manuscript No. JDAR-23-86260 (R); Published: 30-Jan-2023, DOI: 10.4303/JDAR/236216
Abstract
Background: Left Ventricular End Systolic Volume (LVESV) is one of the parameters to assess left ventricular function other than ejection fraction. The LVESV value is an indicator of remodelling after myocardial necrosis and has been shown to have prognostic value in post-infarction patients. Research on the relationship between end systolic volume and mortality or major cardiovascular events has been carried out in post-infarction patients. Similar studies in the population of stable angina pectoris have not been widely carried out.
Objective: To determine the prognostic role of LVESV in predicting major cardiovascular events (MACE) and determine the median LVESV value that can predict MACE in patients with stable CHD.
Research methods: The study was conducted using a retrospective cohort method on 103 stable CHD patients without a history of infarction or revascularization who underwent SPECT Tc99m tetrofosmin examination at the nuclear department of the Harapan Kita National Heart Center from January 2017 to June 2018 which will be followed for 6 months unless MACE occurs.
Results: The numbers of subjects analyzed in this study were 103 patients. During the observation period there were a total of 29 patients (28.2%) who experienced major cardiovascular events. Patients who experienced MACE had a higher LVESV value (190.31 ± 115.63 mL vs 105.76 ± 80.44 mL) when compared to patients who did not experience MACE (p=0.001). The results of the bivariate analysis showed that the final systolic volume was statistically significant. The results of cox regression analysis showed that the final systolic volume value of ≥ 113mL was a predictor of major cardiovascular events in patients with stable coronary heart disease with hazard ratio 3,753 (CI 1.595-8,855; p value=0.001).
Conclusion: End systolic volume (ESV) is one of the significant independent predictors of MACE. The value of the end systolic volume (ESV) of ≥113 mL has a predictor value for the occurrence of MACE.
Keywords
End systolic volume; Coronary heart disease; Major adverse cardiovascular events
Introduction
End Systolic Volume (ESV) is one of the parameters to assess left ventricular function in addition to ejection fraction. The ESV value is an indicator of remodelling after myocardial necrosis and has been shown to have prognostic value in post-infarction patients [1]. Sharir et al. reported that end systolic volume measured by SPECT (Single Photon Emission Computed Tomography) >70 ml was associated with high mortality within 6 months post-infarction [2].
White et al. reported the results of a study in 605 post-infarct patients, who were followed for 78 ± 32 months, showing that end systolic volume ≥ 100 mL had a higher mortality when compared to patients with end systolic volume <100 mL and was the best predictor of good prognosis compared with end-diastolic volume and ejection fraction [1].
Yao et al. demonstrated that increased ESV during peak stress echocardiography is a marker of severe and extensive coronary disease, and associated with an increased risk of cardiovascular events in patients with known coronary heart disease [3]. Sinaga et al. stated that stable coronary heart disease patients with ESVI cut-off point ≥ 22 ml/m2 are having predictive value for the occurrence of MACE [4].
Research on the relationship between end systolic volume and mortality or major adverse cardiovascular events has been carried out in post-infarction patients. However, similar studies in the population of stable angina pectoris have not been widely carried out.
Methods
This study was conducted using a retrospective cohort method by taking secondary data from the registry of 103 stable CHD patients without any history of infarction or revascularization who underwent SPECT Tc99m tetrofosmin examination in the nuclear section of the Harapan Kita National Heart Center from January 2017 to June 2018. All patients were observed for 6 months unless MACE occurs.
Data were collected on all patients with known or suspected coronary heart disease, who underwent the SPECT Tc99 tetrofosmin examination from January 2017-June 2018 and were screened according to the inclusion and exclusion criteria. The results of the SPECT Tc99m tetrofosmin examination after adenosine stress were obtained; the results of left ventricular function parameters (ejection fraction and end systolic volume) were examined. Patients were observed until the end of December 2018, for at least 6 months after the SPECT examination. Patient data regarding MACE was taken from status, confirmed by telephone interview, or letter correspondence.
SPECT Tc99 tetrofosmin implementation procedure as follows:
• All patients were told to fast for at least 8 hours, delayed beta-blocking drugs and were not to consume caffeinated drinks within 24 hours.
• Pharmacological stress was done with adenosine injection at a rate of 140 micrograms/kgBW/minute for 6 minutes. At the 3rd minute, technetium-99 tetrofosmin was injected intravenously with a dose of 7.5 mCi.
• 30 minutes later, SPECT imaging was acquired with the E-Cam dual-head 3600 gamma camera. The 32 images were taken for 20 seconds each with a 64 × 64 zoom matrix of 1.45, with an initial angle of 54 degrees, up to 104 degrees, using a non-circular orbit.
• For imaging acquisition at rest, an injection of technetium-99 tetrofosmin was performed 3 hours after the first injection at a dose of 15-20 mCi. The process of picture-taking at rest was the same as the process during the stress test.
• Data were reconstructed by tomographic section projections of short-axis and long-axis vertical/horizontal views.
• Myocardial perfusion data, left ventricular volume measurements and left ventricular ejection fraction were performed using the Cedars-Sinai software.
• If the reconstruction and reorientation of boundaries and axes didn’t show good results automatically, then it’s done manually.
Statistical analysis
All continuous variables with a normal distribution are written in the mean of the standard deviation. If the distribution is not normal, the data will be written in the median including the minimum and maximum values. The difference between the two means using the student T test or Mann-Whitney analysis for unpaired variables depends on the normality data distribution. All categorical variables were written in percentage and differences in categorical variables were analyzed by chi-square. Univariate, bivariate and multivariate analysis tests were conducted to obtain factors that play a role in the occurrence of MACE.
To identify predictive variables of MACE, cox proportional hazard regression model is used. Statistical significance was assessed based on p<0.05. Kaplan-Meier method is used to predict life expectancy.
Results
Table 1 shows that 103 patients were analyzed in this study with mean age of 58.61 ± 8.960 years, of which 79 men (76.7%) and 24 women (23.3%). The highest risk factor was hypertension (57.3%) followed by dyslipidemia (56.3%), DM (38.8%), smoking (13.6%) and family history (24.3%). The mean value of SSS, SRS, and SDS are 22.52 ± 13,674; 17.21 ± 13,746; 5.22 ± 4.69 respectively.
Table 1: Baseline characteristics.
| Variable | Total N=103 (100%) | KKVM | Significance (P) | |
|---|---|---|---|---|
| -N=74 (71.87%) | +N=29 (28.2%) | |||
| Age | 58.61 ± 8.960 | 58.04 ± 8.71 | 60.07 ± 9.56 | 0.326 |
| Gender | ||||
| Man | 79 (76.7%) | 56 (70.9%) | 23 (29.1%) | 0.695 |
| Woman | 24 (23.3%) | 18 (75%) | 6 (25%) | 0.695 |
| Risk factor | ||||
| Hypertension | 59 (57.3%) | 38 (64.4%) | 21 (35.6%) | 0.052 |
| DM | 40 (38.8%) | 27 (67.5%) | 13 (32.5%) | 0.435 |
| Dyslipidemia | 58 (56.3%) | 40 (69%) | 18 (31%) | 0.461 |
| Smoke | 35 (34%) | 24 (68.6%) | 11 (31.4%) | 0.596 |
| Obesity | 14 (13.6%) | 8 (57.1%) | 6 (42.9%) | 0.188 |
| Family history | 25 (24.3%) | 16 (64%) | 9 (36%) | 0.316 |
| Perfusion myocardial | ||||
| SSS | 22.52 ± 13.674 | 21.65 ± 14.03 | 24.76 ± 12.67 | 0.282 |
| 17.21 ± 13.746 | ||||
| SRS | 5.22 ± 4.69 | 16.20 ± 14.12 | 19.79 ± 12.79 | 0.219 |
| SDS | 5.45 ± 4.91 | 4.66 ± 4.11 | 0.411 | |
| Stress left ventricular function | ||||
| EF Stress | ||||
| VDA | 34 (9-86) | 38 (10-86) | 20 (9-85) | 0.016 |
| 177.75 ± 103.41 | 153.35 ± 83.95 | 240 ± 122.47 | 0.001 | |
| VSA | 129.56 ± 98.81 | |||
| (4-453) | 105.76 ± 80.44 | 190.31 ± 115.63 | 0.001 | |
| 75.19 ± 57.99 | ||||
| IVSA | 103.07 ± 60.09 | |||
| IVDA | 61.08 ± 46.87 | 111.20 ± 66.66 | 0.001 | |
| 88.42 ± 48.42 | 140.46 ± 70.90 | 0.001 | ||
From the post-stress examination of left ventricular function, the mean value of the ejection fraction when stressed was 34 (9-86), the EDV value was 177.5 ± 103.41, the ESV value was 129.56 ± 98.81, the ESVI value was 75.19 ± 57.99, and the EDVI value was 103.07 ± 60.09.
During the observation period, there were total of 29 patients (28.2%) who experienced major adverse cardiovascular events. Patients who experienced MACE had higher ESV value (190.31 ± 115.63 mL vs 105.76 ± 80.44 mL) when compared to patients who did not experience MACE (p=0.001). Additionally, MACE was more common in patients with lower stress ejection fraction (20% vs 38%), higher EDV, higher ESVI and higher EDVI values. Table 2 shows results of the bivariate risk factors test for major adverse cardiovascular events found hypertension, diabetes mellitus, dyslipidemia, smoking, obesity, and family history played clinical role in increasing MACE in patients with stable coronary heart disease but these results were not statistically significant (p>0.05).
Table 2: Bivariate analysis.
| Variable | OR | 95% CI | P value |
|---|---|---|---|
| Hypertension | 2,022 | 0.838–4.877 | 0.114 |
| DM | 1,346 | 0.576–3.147 | 0.492 |
| Dilipidemia | 1,199 | 0.514–2.795 | 0.674 |
| Smoke | 1,524 | 0.641–3.624 | 0.339 |
| Obesity | 1,817 | 0.574–5.766 | 0.305 |
| Family History | 1.35 | 0.520–3.480 | 0.54 |
| Perfusion myocardial | |||
| SSS ≥ 14 | 0.51 | 0.202–1.299 | 0.155 |
| Post Stress EF<56% | 0.36 | 0.113–1.172 | 0.082 |
| LVESV ≥ 113 | 4,610 | 1.749–12.146 | 0.001 |
| ESVI ≥ 22 | 3,532 | 0.963–12.955 | 0.046 |
Bivariate analysis shows a median end systolic volume of ≥ 113 mL as a predictor of major adverse cardiovascular events in patients with stable coronary heart disease with HR 4.61 (CI 1.749-12,146; p value 0.001). Cox regression analysis in Table 3 shows ESV ≥ 113 mL as a predictor of major adverse cardiovascular events in patients with stable coronary heart disease with HR 3,753 (CI 1.595-8,855; p value=0.001).
Table 3: COX analysis of LVESV regression with MACE.
| HR | 95% CI | P | |
|---|---|---|---|
| LVESV 113 | 3,753 | 1.595–8.855 | 0 |
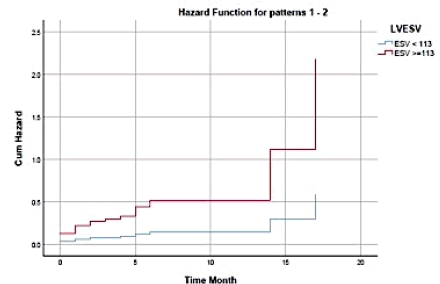
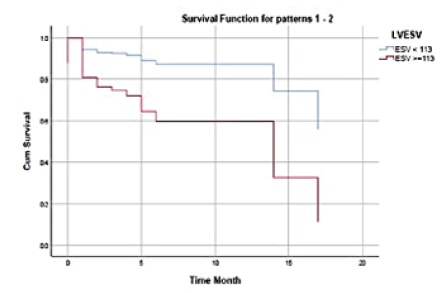
Based on the graph in Figures 1 and 2, it was found that the number of samples who died with a final systolic volume value of ≥ 113 mL was around 29 people. In ESV ≥ 113 mL, the highest number of MACE events was found in the mean follow-up for the first 5 months. This data shows the end systolic volume of ≤ 113 mL has better prognostic value in 20 months of observation in patients with stable coronary heart disease.
Figure 1: Kaplan Meier LVESV graph by survival rate.
Figure 2: Kaplan Meier LVESV graph and hazard ratio.
Discussion
Determination of left ventricular systolic and diastolic function is a very important clinical parameter for the diagnosis process, therapy selection, and patient evaluation with heart disease. In clinical practice, the most frequently measured parameters to determine left ventricular function are end systolic volume, end diastolic volume, cardiac output, and ejection fraction. End systolic volume is the volume of blood in the left ventricle at the end of the systolic phase. The relationship between end systolic volume and mortality or major adverse cardiovascular events has not been widely studied instable angina pectoris population, whereas end systolic volume is associated with left ventricular dilatation due to expansion of ischemia and ventricular dilation due to scar tissue. Thus, end systolic volume may be a more significant predictor of prognosis than ejection fraction in assessing major cardiovascular events or death instable angina pectoris [1].
The value of the ESV examination varies greatly, as can be seen from the standard de tion which exceeds mean value. This indicates the magnitude of the ESV variation in CHD patients who have not had myocardial infarction, and associated with variations degree of ischemia suffered by the subjects.
In this study, the mean ESV value was 129.56 mL ± 98.81 mL, with the smallest ESV value of 4 mL and the largest ESV value of 453 mL, was found. The normal range for ESV and EDV in the normal population as published by Kakhki et al. was 11.4 mL ± 7.2 mL and 48.8 ± 14.3 mL in women and 27.9 mL ± 13.7 mL and 76 mL ± 27.2 mL in men [5].
Bivariate analysis from SPECT examination, namely parameters EDVI ≥ 92 ml/m2, ESV ≥ 113 mL, and ESVI ≥ 22 ml/m2 had a significant value on MACE. This study shows that the ESV value of ≥ 113 mL has predictive value for the occurrence of MACE. White et al. in their study found that the end systolic volume was the main predictor in assessing survival in myocardial infarction patients with ESV cutoff value >100 mL [1]. Sharir et al. demonstrated that end systolic volume has significant prognostic value in predicting cardiac death and can be clinically useful in risk stratification. In the study, conducted by Norris et al., found that the left ventricular end systolic volume obtained from echocardiography is an opposing prognostic factor that affects the healing process in patients with myocardial infarction and strong predictor in assessing cardiac mortality [6]. A previous study by Burns et al. concluded that an increase in the end systolic volume value in patients with acute myocardial infarction was associated with increase in mortality, suggesting that greater end systolic volume value in patients with coronary heart disease is an important predictor of major adverse cardiovascular events [7].
The study from McManus et al. showed that ESVI >25 mL/m2 was an independent predictor of hospitalization in heart failure patients with stable coronary heart disease [8]. Kato et al. mentioned that ESVI is a prognostic indicator in heart failure patients with preserved ejection fraction (HR: 1.049, 95% CI: 1.025-1.074, P<0.001) [9]. Sinaga et al. concluded that left ventricular end systolic volume index was an independent predictor for the occurrence of MACE. The ESVI cut point of ≥ 22 ml/m2 has predictive value for the occurrence of MACE [4].
Conclusion
End systolic volume (ESV) is an independent predictor for the occurrence of MACE. The value of the end systolic volume (ESV) of ≥ 113 mL has predictive value for the occurrence of MACE.
Acknowledgement
None.
Conflict of Interest
Authors have no conflict of interest to declare.
References
- H.D White, R.M. Norris, M.A. Brown, P.W. Brandt, R.M.L. Whitlock, et al. Left ventricular end-systolic volume as the major determinant of survival after recovery from myocardial infarction, Circulation, 76(1987):44-51.
- T. Sharir, G. Germano, P.B. Kavanagh, S. Lai, I. Cohen, et al. incremental prognostic value of post-stress left ventricular ejection fraction and volume by gated myocardial perfusion single photon emission computed tomography, Circulation, 100(1999):1035-1042.
- S.S. Yao, A. Shah, S. Bangalore, F.A. Chaudhry, Transient ischemic left ventricular cavity dilatation is a significant predictor of severe and extensive coronary artery disease and adverse outcome in patients undergoing stress echocardiography, J Am Soc Echocardiography, 20(2007):352-358.
- D.A. Sinaga, Indeks volume sistolik akhir ventrikel kiri paska stress sebagai prediktor independen kejadian kardiovaskular mayor pada pasien penyakit jantung koroner stabil, Universitas Indonesia 2011.
- V.Rd. Kakhki, S.R. Zakavi, R. Sadeghi, M.E. Emadzadeh, A. Vejdani, Normal values of left ventricular functional indices in gated 99 mtc-mibi myocardial perfusion SPECT, Iran J Nucl Med, 16(2008):14-19.
- R.M. Norris, H.D. White, D.B. Cross, C.J. Wild, R.M.L. Whitlock, Prognosis after recovery from myocardial infarction: The relative importance of cardiac dilatation and coronary stenoses, Eur Heart J, 13(1992):1611-1618.
- R.J. Burns, R.J. Gibbons, Q. Yi, R.S. Roberts, T.D. Miller, et al. The relationships of left ventricular ejection fraction, end-systolic volume index and infarct size to six-month mortality after hospital discharge following myocardial infarction treated by thrombolysis, J Am Coll Cardiol, 39(2002):30-36.
- D.D. McManus, S.J. Shah, M.R. Fabi, A. Rosen, M.A. Whooley, et al. Prognostic value of left ventricular end-systolic volume index as a predictor of heart failure hospitalization in stable coronary artery disease: Data from the heart and soul study, J Am Soc Echocardiogram, 22(2009):190-197.
- M. Kato, S. Kitada, Y. Kawada, S. Kikuchi, O. Nobuyuki, Importance of left ventricular end-systolic volume index as a prognostic indicator in heart failure with preserved left ventricular ejection fraction, JCF, 23(2017):S16
Copyright: © 2023 Hilfan AP Lubis, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium provided the original work is properly cited.