Case Report - Journal of Drug and Alcohol Research ( 2024) Volume 13, Issue 1
Megadose Methylprednisolone in Acute Traumatic Spinal Cord Injury
Yehezkiel Kurniawan1, Yudhisman Imran2,3*, Mulia Rahmansyah4,5, Irmiya Rachmiyani6, Triasti Khusfiani7, Ainaya Az Zahra8 and Emad Yousif92Department of Neurology, Universitas Trisakti, Indonesia
3Department of Neurology, Hermina Daan Mogot Hospitals, Indonesia
4Department of Radiology, Universitas Trisakti, Indonesia
5Department of Radiology, Hermina Daan Mogot Hospitals, Indonesia
6Department of Obstetrics and Gynecology, Universitas Trisakti, Indonesia
7Department of Pharmacology, Universitas Trisakti, Indonesia
8Medical Education Study Programme, Universitas Trisakti, Indonesia
9Department of Chemistry, Al-Nahrain University, Iraq
Yudhisman Imran, Department of Neurology, Universitas Trisakti, Indonesia, Email: yudhisman.imran@trisakti.ac.id
Received: 03-Jan-2024, Manuscript No. JDAR-24-126284 ; Editor assigned: 05-Jan-2024, Pre QC No. JDAR-24-126284 (PQ); Reviewed: 19-Jan-2024, QC No. JDAR-24-126284; Revised: 24-Jan-2024, Manuscript No. JDAR-24-126284 (R); Published: 31-Jan-2024, DOI: 10.4303/JDAR/236276
Abstract
Methylprednisolone (MP) has neuroprotective and anti-inflammatory effects at the cellular level in cases of acute traumatic Spinal Cord Injury(SCI). A 27-year-old man was referred to the emergency room because unable to move both limbs since 4.5 hours ago after falling down from a height of 3 meters. In the Neurology examination was found lower limb motor strength (0000/0000). Thoracolumbar X-ray showed wedge-shaped compression with vertebral body retropulsion of Lumbar1. Patient received an intravenous megadose MP and kyphoplasty surgery and stabilization of the L1 vertebral corpus. After treatment, the patient’s motor strength improved to 5555/5555. During treatment, the patient did not complain of heartburn, or tightness and no decubitus ulcers were found. This case report emphasizes the effective use of megadose MP in acute traumatic SCI but underscores the importance of careful consideration of the risk- benefit profile, monitoring of side effects, and the timing of administration.
Keywords
Methylprednisolone; Megadose; Spinal cord injury; Steroid
Introduction
Spinal Cord Injury (SCI) is a temporary or a permanent damage to the spinal cord, which can be caused by a non-traumatic or traumatic events [1,2]. Causes of nontraumatic SCI includes vascular insufficiency, malignancy, osteoarthritis, or infections such as tuberculous spondylitis and abscess or paraspinal edema that can cause spinal cord compression [1,3]. In traumatic SCI, the most common causes are fractures, traffic accidents, falls from height, or acts of violence [2,4].
According to WHO (World Health Organization) data in 2013, every year around 250,000-500,000 people experience spinal cord injury, and the estimated global incidence is 40 cases-80 cases per one million population which 90% of these cases are due to trauma [5]. Traumatic spinal cord injury can cause neurological deficits whose clinical features vary depending on the severity and location of the lesion in the spinal cord, such as paralysis, hypoesthesia, paresthesia, spasticity, pain, as well as cardiovascular, digestive, urinary, or sexual dysfunction [1,4]. An Immediate Management of acute SCI is very important after an injury, so that the decreased neurological function can be recovered more quickly [1]. One of the therapies that can be given immediately is corticosteroids as an anti-inflammatory, for example, Methylprednisolone [1].
At the cellular level, methylprednisolone has been shown to reduce lipid peroxidation, apoptosis, and control the inflammatory response in acute spinal cord injury [6]. The use of megadose methylprednisolone has its pros and cons because of the higher potential side effects, and according to some studies only provide minimal or no clinical improvement [6]. There is also an increased risk of adverse events (e.g. respiratory tract infection, gastrointestinal bleeding, wound infection, hyperglycemia) with high-dose MP regimens over 48 hours, but there is a lower complication rate when high-dose MP is given over 24 hours and still provides neurological improvement [6,7].
This case report presents a patient with an acute traumatic SCI experiencing clinical improvement and minimal adverse events following 48 hours of megadose MP at an onset of injury of less than 8 hours.
Illustration of Case
A 27-year-old man was referred from his previous hospital to the emergency room of Hermina Daan Mogot Hospital for vertebrae surgery. The patient’s main complaint was unable to move both limbs since 4.5 hours ago after falling down from a height of 3 meters. This incident occurred when the patient was about to install CCTV on the ceiling. After falling, the patient felt pain in the lower back, could not move from the waist down to both legs and felt a tingling sensation from the abdomen to the tips of the toes. Decreased consciousness and head impact were denied.
Vital signs examination showed blood pressure 113 mmHg/80 mmHg, pulse 80 beats/min, respiration 20 beats/ min, body temperature 36.5oC, oxygen saturation 98%. There was no impairment found on physical examination, other generalist status was within normal limits.
Upper limb motor strength (5555/5555), lower limb motor strength (0000/0000), arm physiological reflexes within normal limits, patella (+3/+3) and achilles (+3/+3). Sensory examination obtained hypoesthesia as high as thoracic dermatome 9 (T9). cranial nerve examination within normal limits, meningeal excitatory sign examination was not performed.
Routine blood laboratory examination was performed with the results of leukocytes 12,100 103/uL and mild hypokalemia 3.24 mmol/L. Other blood laboratory examinations such as renal function, current blood and hemostasis were within normal limits. Thoracolumbar X-ray showed wedge-shaped compression with vertebral body retropulsion of Lumbar 1 (L1) with kyphotic curve which correlate with hyperflexion injury (Figure 1). Computed tomography scan (CT scan) of the brain with bone window (Figure 2), as well as cervical X-ray did not show any abnormalities.
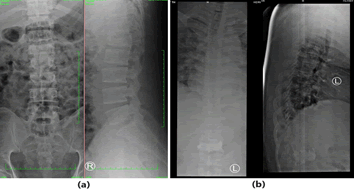
Figure 1: Thoracolumbar X-Ray of AP and lateral position, (a) Day one (Pre-Kyphoplasty), compression fracture with retropulsion (Red circle), (b) Day four (Post-Kyphoplasty), mild deformity post-cement vertebroplasty (Blue circle)
The working diagnosis is paraplegia upper motor neuron (UMN) hypoesthesia as high as dermatome T9 et causa spinal cord trauma segment T9 and L1 vertebra corpus compression fracture.
Management on the 1st day, the patient received an Intravenous (IV) Methylprednisolone (MP) in the emergency room at a dose of 30 mg/kgBB for 15 minutes, after completion then continued 45 minutes later with a dose of MP 5.7 mg/kgBB for 47 hours. The patient was also given Ketorolac 30 mg IV and Pregabalin 75 mg orally every 12 hours as an anti-pain management. The patient was given Omeprazole 40 mg/12 hours IV given as a gastroprotector, lactated Ringer fluid therapy 500 ml/24 hours and a folley catheter installation.
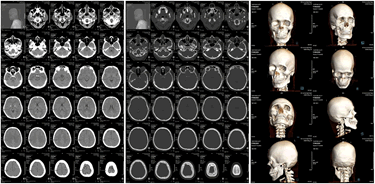
Figure 2: CT scan of the head and bone window within normal limits
On the 2nd day of treatment, the patient complained that there was no urge to urinate, could not defecate and could not have an erection. On neurological examination, the patient’s lower extremity motor strength improved to (4433/3344), sensory examination: Hypoesthesia as high as T9 dermatome, and physiological reflexes of patella and achilles (+3/+3). On this 2nd day, kyphoplasty surgery and stabilization of the L1 vertebral corpus compression fracture were performed by an orthopedic surgeon subspecializing in spine.
On the 3rd day of treatment, there was an improvement in the patient’s lower extremity motor strength to (5444/4445), and sensory improvement to hypoesthesia as high as dermatome T11-T12, physiological patellar and Achilles reflexes were still (+3/+3). Methylprednisolone administration was completed on this day.
On the 4th day of treatment, the patient’s sensory neurology physical examination had no improvement, autonomic examination still obtained alvi retention, but motor strength improved to (5544/4455). Routine blood laboratory examination was carried out for follow-up and the results obtained were 14,150 103/uL leukocytes, 159 mg/dl current blood glucose, as well as post kyphoplasty thoracolumbar x-rays. The patient was able to stand up but still felt pain in the lower back, Tramadol 50 mg/12 hours IV and Amitriptyline 25 mg/12 hours orally was then given as an additional therapy.
On the 5th day of treatment, the patient’s motor strength examination has improved to (5554/4555), and sensory improvement to hypoesthesia as high as the L1 dermatome, physiological reflexes of the patella and achilles are still (+3/+3), the patient has start to feel the urge to urinate, but still no defecation. Fleet enema was given to overcome the symptoms of constipation, and physiotherapy was planned as a non-pharmacological therapy.
On the 6th day of treatment results from a thoracal Magnetic Resonance Imaging (MRI) examination without contrast Post Kyphoplasty and Stabilization showed a mild deformity with bone-cement post vertebroplasty at the vertebra body of L1, without osteomyelitis, retropulsion of vertebra body of L1 still seen and also bulging disc of T12-L1 and L1-L2 showed with mild thoracolumbar canal stenosis. The patient also had a blood glucose test, with a result of 102 mg/dl (Figure 3).

Figure 3: Magnetic Resonance Imaging (MRI) of the thoracal without contrast of the patient. (Description: Circle: Post-cement vertroplasty deformity, blue arrow: Retropulsion of L1 with mild canalis lumbar stenosis)
On the 7th day of treatment, the patient’s motor strength improved to (5555/5555), hypoesthesia sensory examination as high as the L1 dermatome, and physiological patella and achilles reflexes (+3/+3). During treatment, the patient did not complain of heartburn, or tightness and no decubitus ulcers were found. The patient was discharged with a folley catheter still attached.
The patient returned to a neurologist on the 14th day with autonomic complaints, namely still unable to have an erection and unable to feel when defecating. Motor strength examination was within normal limits. Sensory examination still obtained hypoesthesia as high as L1 dermatome.
Discussion
Spinal cord injury can cause persistent neurological deficits, and the clinical course varies depending on the level of injury location and the amount of spinal cord tissue that is still intact [2,8]. Spinal cord injury generally occurs as a result of trauma to the vertebrae resulting in damage to the spinal cord or disruption of surrounding structures such as bone, ligaments and blood vessels [8].
Spinal cord injury is divided into 2 phases, namely primary and secondary injury. The initial stage immediately after trauma is known as primary injury, generally due to compression of the spinal cord structures, either by bone fragments, intervertebral disc herniation, or the process of hematoma accumulation in the spinal cord itself, causing symptoms in the form of neurological deficits or pain [2,8,9]. Other mechanisms due to the mechanical force of trauma can include penetrating wounds, stretching, and tearing of the spinal cord structures and blood vessels [1]. This primary injury phase includes spinal cord parenchyma destruction, axon network disruption, hemorrhage, and glia membrane damage [8]. The extent of damage and duration of spinal cord compression at the onset of trauma is a major determinant of injury severity [8].
The various things that happen in the primary injury will trigger the secondary injury phase, which is a series of biochemical, mechanical, and physiological changes in the spinal cord [8]. This secondary injury is also divided into three phases: Acute, sub-acute, and chronic [4,8]. The pathological changes that occur in acute secondary injury are increased cell permeability, ion dysregulation, excitotoxicity, free radical production, lipid peroxidation, increased calcium flow, inflammation, edema, and necrosis [8]. If this continues, a sub-acute secondary injury phase will begin, characterized by features such as neuronal apoptosis, axon demyelination, Wallerian degeneration, axon remodeling, and glial scar tissue formation [1,8]. The sub-acute phase leading to the chronic phase is characterized by cystic cavity formation, axon death, and glial scar tissue maturation [8].
This series of injuries can lead to decreased or loss of motor and sensory functions originating below the level of injury [2]. Loss of sensorimotor function in all four extremities is called tetraplegia or quadriplegia, while when it occurs in both lower limbs it is called paraplegia [1].
In this case the patient had a traumatic spinal cord injury. The primary injury occurred when the patient fell down from a height of three meters. After the primary injury, there was hypoesthesia as high as T9 dermatome, paraplegia (0000/0000), and increased physiological patellar and achilles reflexes (+3/+3).
The International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI), developed by the American Spinal Injury Association (ASIA), is often used to assess the severity of injury. The severity of the injury is classified into degrees in the ASIA Impairment Scale (Table 1) [1,4,10].
Table 1: ASIA impairment scale
| American Spinal Injury Association (ASIA) impairment scale | ||
|---|---|---|
| Grade | Type of injury | Description of injury |
| A | Complete | Loss of motor and sensory function below the injured segment of the spinal cord, including S4-S5 (no sacral sparing). |
| B | Uncomplete | Loss of motor function below the injured segment. Variable loss of sensory function below the injured segment, there is sacral sparing at S4-S5. |
| C | Uncomplete | Loss of motor function >50% below the injured segment. Motor strength of the affected muscle <3, unable to resist gravity. |
| D | Uncomplete | Loss of motor function <50% below the injured segment. Motor strength of the affected muscle = 3, can resist gravity. |
| E | Normal | Normal motor and sensory functions. |
The patient fit into the ASIA impairment scale grade A category because immediately after the primary injury, the patient had paraplegia, hypoesthesia as high as the T9 dermatome, no sacral sparing, and was unable to urinate and defecate.
X-ray examination, CT scan and MRI are commonly used radiologic examinations to look at spinal cord damage and injury [2]. X-ray examination is used to identify the presence or absence of fractures such as wedge compression fracture, burst fracture, or dislocation of the vertebrae after spinal cord trauma [1,2]. In this patient, a lumbosacral X-ray was performed, and showed a wedge-shaped compression of the vertebrae body of L1 without listhesis.
From the neurological examination and lumbosacral X-ray, secondary acute-phase injury such as edema or hematoma of the T9 vertebra was suspected. In this case, a followup MRI is needed to identify spinal cord transection and evaluate for edema and/or haemorrhage [2].
After a thoracic MRI without contrast, the results showed a compression fracture with retropulsion of the vertebra body of L1; bulging discs T12-L1 and L1-L2 with mild thoracolumbar canal stenosis; intravertebral disc herniation (Schmorl’s node) at level T9, T11 and T12; post-cement vertebroplasty deformity of the vertebral body of L1 (Figure 3).
Radiological examination results in lumbosacral x-rays and thoracic MRI without contrast showed posterior compression of the vertebral body L1 and bulging discs of T12-L1 and L1-L2 compressed anterior thecal sac support the neurological clinical findings found, namely the presence of autonomic disorders unable to urinate and defecate.
The diagnosis was paraplegia Upper Motor Neuron (UMN) hypoesthesia as high as dermatome T9 et causa spinal cord trauma T9 segment and compression fracture of vertebral body L1.
Urinary tract infections, cardiopulmonary problems, neuropathic pain and decubitus ulcers are the most common complications in spinal cord trauma patients if the patient’s condition requires prolonged bed rest [7,11]. These complications can increase morbidity, prolong hospital stays, and interfere with important rehabilitation or physiotherapy [11]. Therefore, prevention of complications plays a very important role in the patient’s prognosis. The goal of rehabilitation in spinal cord injury is to reduce disability and minimize limitations, by trying to increase range of motion. This patient is also recommended for physiotherapy, so that daily life activities can be carried out as much as possible.
Corticosteroids
The use of corticosteroids in acute SCI patients began in 1960 with the idea that the anti-inflammatory effects of corticosteroids would reduce spinal cord edema based on the experience of steroid use in cerebral edema [12]. Corticosteroids consist of 2 classes, glucocorticoids and mineralocorticoids, but the term “corticosteroid” generally refers to the glucocorticoid class [13]. In general, mineralocorticoids primarily regulate sodium and fluid levels, while glucocorticoids regulate a variety of cellular functions including growth and development, cognition, metabolism, homeostasis and inflammation [6,13].
Corticosteroids are known to have neuroprotective effects, including improving vascular perfusion, preventing calcium influx and accumulation, modulating inflammatory cells, preventing spinal cord neurofilament protein loss, facilitating neuronal excitability and impulse conduction, inhibition of inflammatory cytokines and inhibition of lipid peroxidation [8,12]. The acute inflammatory response at the site of spinal cord injury and hemorrhage can result in the production of Reactive Oxygen Species (ROS) and cytotoxic edema, which contribute to lipid peroxidation and ischemia [14]. Lipid peroxidation is a highly damaging reaction to central nervous cell membranes. This reaction can independently and progressively spread to surrounding healthy cells [4]. Because central nervous cell membranes contain relatively large amounts of fatty acids, the central nervous system is particularly susceptible to large amounts of lipid peroxidation, which can eventually lead to demyelination and neurodegeneration [4,14]. Inhibitory effects of lipid peroxidation are the strongest neuroprotective characteristics of corticosteroids [12]. Dexamethasone and Methylprednisolone are 2 synthetic glucocorticoids commonly used in the management of central nervous system pathologies [6].
In cases of cerebral edema such as due to tuberculous meningitis or intracranial neoplasms, the steroid given is dexamethasone because it has very low mineralocorticoid activity, a long half-life, and high effectiveness [15,16]. The role of dexamethasone in cerebral tumors with edema is to reduce the expression of Vascular Endothelial Growth Factors (VEGF) thereby improving blood brain barrier dysfunction [15]. In the administration of dexamethasone 16 mg for 2 days showed a decrease in cerebral edema volume by 1.7% compared to before dexamethasone administration [15].
Dexamethasone also has lipid anti-oxidation activity, but is slightly less effective than Methylprednisolone [14]. Unlike dexamethasone, methylprednisolone has the ability to bind to mineralocorticoid receptors which can produce sodium retention effects [6]. Methylprednisolone can prevent increased spinal cord blood flow, prevent post-traumatic spinal cord neurofilament ischemia and degeneration, enhance energy metabolism, restore extracellular calcium, and improve nerve impulse conduction [1,14]. Methylprednisolone also inhibits ROS synthesis, free fatty acid release, and as a result inhibits tissue lipid peroxidation [8,14]. As a result, MP can reduce the lesion volume in spinal cord contusion and suppress vasogenic edema with inflammatory response [14]. In cases of edema due to acute spinal cord injury, Methylprednisolone is a more effective corticosteroid than other glucocorticoids [12].
This patient with an onset of 4.5 hours received megadose MP at a dose of 30 mg/kgBB for 15 minutes, then continued 45 minutes later at a dose of 5.7 mg/kgBB for 47 hours. The patient experienced clinical improvement in motor and sensory strength gradually from the 1st day to the 7th day of treatment. Improvement in motor strength has occurred on the second day before surgery, this can be considered due to reduced edema in the T9 spinal cord due to the administration of megadose methylprednisolone since the 1st day. On sensory examination, the patient’s hypoesthesia dropped from the level of T9 dermatome to L1 dermatome. While on thoracic MRI examination, it was found that at L1 there was posterior compression of the vertebral body L1 (retropulsion) and bulging discs T12-L1 and L1-L2 that compressed anterior thecal sac with mild thoracolumbar canal stenosis. This indicates that the structural abnormality is at L1, not T9.
At the time of control on the 14th day the patient had no motoric complaints, on sensory examination hypoesthesia was found as high as the L1 dermatome and autonomic disorders such as inability to have an erection and no feeling of defecation (Table 2).
Table 2: Improvement of patients' neurologic deficits
| Day | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 14 |
|---|---|---|---|---|---|---|---|---|
| Motoric | 1111/1111 | 4433/4433 | 5444/4445 | 5544/4455 | 5554/4555 | 5554/4555 | 5555/5555 | 5555/5555 |
| Hypoesthesia | T9 | T9 | T11-T12 | T11-T12 | L1 | L1 | L1 | L1 |
| Physiological limb reflexes | 1 | 1 | 1 | 1 | 1 | 1 | 1 | (n) |
| Retention of uri et alvi | Observation | Positive | Positive | Positive | Positive | Positive | Positive | Positive |
Injuries at or above L1-L2 can disrupt the innervation of the vesica urinaria and uri sphincter muscles, which can lead to inability to empty the vesica urinaria, acontractile vesica urinaria and urinary incontinence [2]. If the injury occurs above T11, it may affect psychogenic arousal (i.e., erection or vaginal lubrication due to stimulation of the brain) while maintaining reflexive arousal (i.e., erection or vaginal lubrication due to stimulation of the genitalia) [2]. Injury to the lumbosacral area may also impair voluntary control of the sphincter ani, and/or parasympathetic innervation of the bowel [2].
Historically, the most controversial issue in the management of spinal cord injury has been the appropriateness of administering high doses, or megadoses, of Methylprednisolone Sodium Succinate (MPSS) intravenously in acute phase injury [2]. Currently, the administration of corticosteroids in patients with spinal cord injury is still controversial due to the serious side effects that can occur when administered in high doses [8]. These side effects include respiratory tract infection, gastrointestinal bleeding, wound infection, and hyperglycemia [6,7]. In addition, there are several studies that conclude that MP administration has moderate quality evidence of benefit, and the risk of MP side effects is greater than the neurological benefits [17,18]. In this patient there were no side effects of corticosteroids, except for slightly elevated blood glucose. The patient’s baseline blood glucose was 159 mg/dL during MP administration; 2 days later, the patient’s glucose was 102 mg/dL.
In preclinical evaluation, MPSS showed great potential as a neuroprotective agent.2 Further clinical evaluation of MPSS administration after SCI resulted in three largescale multicenter double-blinded randomized clinical trials, namely NASCIS (National Acute Spinal Cord Injury Studies) I, II, and III in 1984, 1990, and 1997 [2,6,12]. In NASCIS II, MPSS administration (initial bolus dose of 30 mg/kg, followed by infusion of 5.4 mg/kg/hour for 23 hours) showed sensory and motor improvement in patients with spinal cord injury onset of 8 hours, either complete or incomplete [7,12]. An increased risk of wound infection and pulmonary embolism was also found in this study, raising concerns about the risk of complications following steroid administration [12]. NASCIS II was the first clinical study to show pharmacologic agents that had an effect on SCI, which became the basis for the use of steroids after SCI, and encouraged research into other neuroprotective agents after SCI [12]. In NASCIS III, patients who received MPSS (initial bolus dose of 30 mg/kg within the first hour, followed by infusion of 5.4 mg/kg/hour for 23 hours or 47 hours) had improved neurologic function after 1 year post SCI, both in the MPSS administration group with an onset of less than 3 hours with infusion for 24 hours, as well as the MPSS administration group within 3 hours-8 hours with infusion for 48 hours [12]. NASCIS II and III guided the administration of MPSS as a standard clinical practice for acute SCI globally [12].
In a secondary analysis, MP administration (onset less than 8 hours) resulted in a 5-point improvement in ASIA motor scores at 6-month follow-up [2]. A 2012 Cochrane review summarizing 6 large studies on MP administration in acute SCI also found an overall 4-point improvement in ASIA motor scores when MP was administered with an 8-hour onset [7]. Overall, administering a 24-hour megadose infusion of MP resulted in a 4-point improvement in ASIA motor scores compared to the no-treatment or placebo group [2].
Conclusion
In cases of spinal cord trauma, neurological and radiological examinations can help to determine the location of mechanical trauma. A thorough and meticulous neurological examination is also very important, because there can be an edema or hematoma that is not visible by radiological examination, but its clinical manifestations can be found through neurological examination.
The patient in this case received a 48-hour megadose MP with an onset of less than 8 hours and kyphoplasty surgery and stabilization of the LI corpus vertebra compression fracture. When coming to the emergency room of Hermina Daan Mogot Hospital, the patient was in a grade A spinal cord injury in the ASIA impairment scale category. During treatment the patient experienced sensory and motor improvement, until the control on day 14 the patient’s motor strength was normal and there was sensory improvement. Patients still experience autonomic disorders such as unable to have an erection and unable to feel when defecating. The patient also experienced slight hyperglycemia which immediately returned to normal after MP administration was completed.
The administration of Megadose MP should be based on careful consideration, namely in the onset of less than 8 hours after spinal cord trauma and if spinal cord edema is expected. Clinicians should also consider possible side effects, so as not to prolong the hospital stay and plan for the patient to begin rehabilitation.
Acknowledgement
None.
Conflict Of Interest
Authors have no conflict of interest to declare.
References
- K. Venkatesh, S.K. Ghosh, M. Mullick, G. Manivasagam, D. Sen, Spinal cord injury: Pathophysiology, treatment strategies, associated challenges, and future implications, Cell Tissue Res, 377(2019):125-51.
- C.S. Ahuja, J.R Wilson, S. Nori, M. Kotter, C. Druschel, et al. Traumatic spinal cord injury, Nat Rev Dis Primers, 3(2017).
- B. Basalamah, B.K. Nabila, Y. Imran, M. Rahmansyah, Tuberculous spondylitis: Significant improvement after early intervention, J Biomed Health, (2020):137-43.
- S.A. Quadri, M. Farooqui, A. Ikram, A. Zafar, M.A. Khan, et al. Recent update on basic mechanisms of spinal cord injury, Neurosurg Rev, 43(2018):425-41.
- Spinal cord injury: Pathophysiology, treatment strategies, associated challenges, and future implications
- J.A. Canseco, B.A. Karamian, D.R. Bowles, M.P. Markowitz, S.L. DiMaria, et al. Updated review: The steroid controversy for management of spinal cord injury, World Neurosurg, 150(2021):1-8.
- L.D. Hachem, C.S. Ahuja, M.G. Fehlings, Assessment and management of acute spinal cord injury: From point of injury to rehabilitation, J Spinal Cord Med, 40(2017):665-75.
- A. Anjum, M.D. Yazid, M. Fauzi Daud, J. Idris, A.M.H. Ng, et al. Spinal cord injury: Pathophysiology, multimolecular interactions, and underlying recovery mechanisms, Int J Mol Sci, 21(2020):7533.
- A. Ogrenci, O. Koban, M. Yilmaz, O. Yaman, S. Dalbayrak, Traumatic sequestrated thoracic disc herniation: A case report, Turk Neurosurg, 29(2018):954-6.
- T.T. Roberts, G.R. Leonard, D.J. Cepela, Classifications in brief: American Spinal Injury Association (ASIA) impairment scale, Clin Orthop Relat Re, 475(2017):1499-504.
- M.H. Gedde, H.S. Lilleberg, J. Abmus, N.E. Gilhus, T. Rekand, Traumatic vs non-traumatic spinal cord injury: A comparison of primary rehabilitation outcomes and complications during hospitalization, J Spinal Cord Med, 42(2019):695-701.
- B.J. Lee, J.H. Jeong, Review: Steroid use in patients with acute spinal cord injury and guideline update, Korean J Neurotrauma, 18(2022):22-30.
- S. Ramamoorthy, J.A. Cidlowski, Corticosteroids: Mechanism of action in health and disease, Rheum Dis Clin North Am, 42(2016):15-31.
- C. Topsakal, F.S. Erol, F.M. Ozveren, N. Yilmaz, N. Ilhan, Effects of methylprednisolone and dextromethorphan on lipid peroxidation in an experimental model of spinal cord injury. Neurosurg Rev, 25(2002):258-66.
- L. Nayak, A.M. Molinaro, K. Peters, J.L. Clarke, J.T. Jordan, et al. The effects of administrated dexamethasone on neurologic assessment in neuro-oncology scale in patients with intracranial tumors. Open Access Maced J Med Sci, 9(2021):349-52.
- D. Septa, Y. Imran, R.Y. Pragono, Diagnosis and treatment of tuberculous meningoencephalitis and toxoplasma encephalitis in positive HIV patient: Case report, J Biomed Health, 5(2022):221-7.
- M.G. Fehlings, J.R. Wilson, L.A. Tetreault, B. Aarabi, P. Anderson et al. A clinical practice guideline for the management of patients with acute spinal cord injury: Recommendations on the use of methylprednisolone sodium succinate, Global Spine J, 7(2017):203S-2011S.
- C.A. Bowers, B. Kundu, J. Rosenbluth, G.W.J. Hawryluk, Patients with spinal cord injuries favor administration of methylprednisolone, PLoS One, 11(2016).
Copyright: © 2024 Yehezkiel Kurniawan, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly.

