Research: Journal of Drug and Alcohol Research (2024) Volume 13, Issue 1
New Hypotheses on the Pathogenesis of Neurosyphillis: A Case Report and Comprehensive Review of the Medical Literature
Lourdes de Fatima Ibanez Valdes*Lourdes de Fatima Ibanez Valdes, Department of Neurology, Walter Sisulu University (WSU), South Africa, Email: lourdesfibanezvaldes@gmail.com
Received: 03-Jan-2024, Manuscript No. JDAR-24-126617; Editor assigned: 05-Jan-2024, Pre QC No. JDAR-24-126617 (PQ); Reviewed: 19-Jan-2024, QC No. JDAR-24-126617; Revised: 24-Jan-2024, Manuscript No. JDAR-24-126617 (R); Published: 31-Jan-2024, DOI: 10.4303/JDAR/236278
Abstract
Background: Neurosyphilis (Ns)-including auditory and ocular forms, is the clinical consequence of infection of the central nervous system by Treponema pallidum (TP). Ns is a Sexually Transmitted Disease (STD) with several stages and development, leading to 6.3 million new infections each year. Up to date the pathogenesis of Ns related to oxidative stress (reactive oxygen species), cytokines, chemokines, mitochondrial activation, and microglial polarization remains unknown. The main aim of this review is to find confident answers the following questions:
- How often is Ns reported in the medical literature of Sub-Saharan Africa?
- What is the most probable pathophysiology of Ns based on the last publications?
Method: We searched the medical literature comprehensively, looking for published Medical Subject Heading (MeSH) terms like "Pathogenesis of neurosyphilis” OR "meningovascular syphilis," OR "syphilitic meningomyelitis" OR "Pathogenesis of secondary syphilis," OR "early secondary syphilis," OR "late neurosyphilis" OR "Immunology of neurosyphilis."
Results: All selected manuscripts were peer-reviewed, and we found only two publications delivering new hypotheses on the pathogenesis of Neurosyphilis (Ns).
Case report: An 18-year-old lady complained of a 5-day history of inability to walk properly due to weakness in her lower limbs and lower back pain. She had no shortness of breath, headache, fever, cough, or difficulty talking. She denies any recent infection or trauma prior to the onset of her symptoms. The final diagnosis of early Ns was confirmed by laboratory investigations on serum and the Cerebrospinal Fluid (CSF) protein level was slightly elevated, and the Treponema pallidum hemagglutination assay and rapid plasma reagin test were positive in both serum and CSF samples.
Comments and concluding remarks: We hypothesized in cases with Ns that the endothelia cell induce a signaling pathway able to modify the cytoskeleton and endothelial junctions at the blood brain barrier, allowing the extravasation of harmful material, which must be removed to the cervical lymphatic chain through the cleaning system composed by the meningeal lymphatic system, glymphatic system, aquaporin 4 and corpus amylacea as we reported for similar situations recently plus an increase expression of almost all before cited elements at the same time.
As far as we know, this is the first article proposing a new hypothesis on the pathogenesis of Ns based on the role played by oxidative stress (reactive oxygen species), cytokines, chemokines, mitochondrial activation, Microglial polarization and many other mentioned proteins and enzymes. As far we know it is the first publication about these novel hypotheses on Ns.
Keywords
Neurosyphillis; Treponema pallidum; Sexually transmitted disease; Penicillin
List of Abbreviations
(AIDS) Acquired Immunodeficiency Syndrome; (CALAS) Cryptococcal Antigen Latex Agglutination System; (CDC) Centers for Disease Control and Prevention; (CN) Cranial Nerve; (CNS) Central Nervous System; (CSF) Cerebrospinal Fluid; (EIA) Enzyme Immunoassay; (FTAABS) Fluorescent Treponemal Antibody Absorption; (HIV) Human Immunodeficiency Virus; (PRISMA) Preferred Reporting Items for Systematic Reviews and Meta- Analyses; (RBC) Red Blood Cells; (RPR) Rapid Plasma Reagin; (TP) Treponema pallidum, (TP-AI) Treponema- Specific Antibody Index; (TPPA) Treponema Pallidum Particle Agglutination Assay; (USA) United States of America; (VDRL) Venereal Disease Research Laboratory; (WBC) White Blood Cells
Introduction
Neurosyphilis (Ns)-including auditory and ocular forms, is the clinical consequence of infection of the central nervous system by Treponema pallidum (TP), which is part of the family of Spirochaetaceae (spirochetes), with a diameter of 0.2 μm and ranging from 6 μm to 15 μm in length. The infection caused by TP causes Syphilis (Sy), which is a Sexually Transmitted Disease (STD) with several stages and development, leading to 6.3 million new infections each year. It is well known that TP penetrates the human body across the injured skin and mucous membranes during sexual intercourse; it is also known that TP has an incomplete biosynthetic pathway, which does not satisfy their requirements for survival in the host. Therefore, they need to get relevant macromolecules during this process while the damaged Vascular Endothelium (VE) allows it to pass into the blood flow and spread all over the body. Last year (Xie and collaborators reported that TP binds to some VE receptors by bacteria adhesion proteins such as Tp0136, Tp0751 and Tp0155 to penetrate the intima of VE and the outer membrane protein of TP is TP)326/Tp92 being the last one who supports the process of attach TP to Endothelial Cell (EC) through cell adhesion.
Nevertheless, vascular injury and abnormal EC are the hallmarks of syphilitic infection [1]. This pathological process has preoccupied many health workers for the past 2 centuries. This pathological process was ubiquitous, and medical doctors recognized it even from the mild clinical manifestations. In South Africa, like many other low and middle-income countries, there has been a resurgence of Syphilis (Sy) apart from certain people in developed countries, but the diagnosis of neurosyphilis tends to be overlooked because of its low frequency [1]. A progressing increment of diagnosed cases of primary and secondary syphilis has been reported in the United States of America every year since 2000, representing 9.5 cases per 100,000 persons in 2017, while in China, 22 cases per 100,000 persons were reported. Ns is rare now, compared to the times before the introduction of therapy with penicillin. On the other hand, rates of Ns have been estimated at 0.47 cases to 2.1 cases per 100,000 population worldwide, and almost half of the cases with early syphilis have been coinfected with HIV, and Ns is found present in twice as many cases with coinfection as persons with free HIV infection [2].
The Center for Disease Control (CDC) in Atlanta establish Ns as
1) any Sy stage and
2) positive CSF VDRL;
Any NS stage, a nonreactive CSF-VDRL, increased CSF protein or WBC count, clinical manifestations consistent with NS without other etiology for this clinical picture [3]. The confirmatory testing in the case of HIV-negative Ns is that of the Fluorescent Treponemal Antibody Testing (FTA-Abs). Other authors had proven that a sensitivity of 90% and 37% specificity when CXCRL12 levels were low and 41% sensitivity and 79% specificity when CXCRL13 levels were high in the absence of associated malignancies, autoimmune disease, or other infections [3,4]. The continued increasing burden of SY could potentially enlarge the pool of people progressing to Ns and Tertiary Syphilis (TS). This transition has been reported in China, where the total reported incidence of Ns and TS also incremented, from 0.02 cases per 100,000 peoples in 2000 to 0.26 cases per 100,000 cases in 2013 [5].
After deleting from the list all misdiagnosed cases, the incidence rate of NS is still elevated [increased from 0.21 cases per 100,000 peoples (202/95,432,604) in 2009 to 0.31 cases per 100,000 peoples (327/106,443,914) in 2014]. Overall, 70.5% of the NS patients received treatment after the diagnosis. However, only 27.1% received the standard treatment [5].
The same authors reported that from 1,968 correctly diagnosed TS, the most common subtype was NS (82.1%), followed by cardiovascular Sy (7.4%, with syphilitic aortitis), skin mucosal membranes (6.1%) and osseous Sy (2.6%). Correctly diagnosed TS patients only accounted for 0.66% (1,968/297,782) of the reported Sy cases during the study period [5].
Sy is a systemic infectious disorder caused by the invasion of the gram-negative spirochete. TP is the only human being’s natural host. Among people aged 15 years-49 years, there are an estimated 6 million new SY cases each year worldwide. According to the National Institute of Public Health of Poland, 1008 new cases of Sy were recorded in 2020 in Poland alone. That group was composed of 29 cases of congenital Sy, 979 cases of early Sy and 550 cases of late Sy, probably related to the elevated number of risky sexual encounters with random people, mainly among homosexual males getting the infection through mucus membranes or broken skin after kisses, sexual intercourse or from mother to fetus via transplacental transmission. Non-sexual syphilitic infection through contact with infected biological material is less frequent. Furthermore, anecdotic cases of Sy due to blood transfusions and transplant transmission have been reported [6].
Syphilitic patients can be grouped into primary and secondary stage early syphilis (within 12 months of infection) and late latent and symptomatic Sy. Since the implementation of penicillin to treat early SY, the number of cases of late symptomatic syphilis has decreased remarkably despite occasional cases of TS still being communicated. As we cited before, late symptomatic syphilis is a highly uncommon systemic disease that can affect the nervous system, the skeletal system mucous membranes, skin, and the circulatory system and very soon after the introduction of penicillin, the incidence of TS dramatically decreased in its early stage, but new cases of this disease are still being reported to the medical literature. Nevertheless, around 25% of untreated patients whose lesions are not infectious and contain an undetectable amount of TP will develop TS, while serum reactions are highly positive. It is also known that one patient can suffer from more than 2 different clinical presentations of this disease. Because the TP pass across the BBB very early, NS manifestation can be seen at any stage of the syphilitic infection. Furthermore, TP has been found in CSF around three weeks after the infection, and the most typical clinical presentations are acute syphilitic meningitis, meningovascular Sy, asymptomatic meningitis, optic neuritis, Sy of the spinal cord, gummas of the CNS, Tabes Dorsalis (TD), neuropsychiatric manifestation, and progressive palsy [6].
Other investigators reported that the Sy global incidence rate is 1.5 cases per 1000 males and 1.5 cases per 1000 females. They divided Sy into 4 stages known as
1) primary;
2) secondary;
3) latent; and
4) tertiary Sy,
each one with associated symptoms and signs characterized by periods of latent infection and episodes of active clinical disease. Despite the clinical course being divided into stages, there is overlap between the stages, and cases may not recollect signs of an earlier disease stage [7]. Other authors confirmed that neurosyphilis can be present at any stage of Sy as well [8,9]. In 2019, Michelle et al. published incidence of Sy was 39.7 cases per 100,000 population, increasing 75% from 2015 [10].
According to Juliet et al. (2022), the incidence of congenital Sy (CS) has dramatically elevated in the USA in the past decade, and it has re-emerged as a familiar neonatal pathogen in American Health Centres despite the remarkable widespread availability of parenteral penicillin. CS is classified as an early or late disease (from birth to 2 years) and commonly manifests within the first 12 weeks of life [11]. Recently, Tanima et al. (2023) reported that a 25-year-old male presented with Optic Neuritis (ON) and documented ON as a new clinical type of presentation of Ns [12]. Garcia and collaborators reported a case presenting an isolated abducent neuritis as a novel manifestation of Ns [13].
The main aim of this study is to answer the following questions:
1. How often is Ns reported in the medical literature of Sub-Saharan Africa?
2. What is the pathophysiology of Ns based on the most recent publications?
Methodology
A systematic search of EMBASE, Medline, Cochrane Library, Scopus, and CINAHL was conducted to identify articles published between January 31st, 2000, and September 30th, 2023, followed by hand-searching relevant journals.
Literature search strategy for this review
A systematic online search of investigations published from January 01st 2000 to January 31st, 2023, was conducted using the following databases: Scopus/PubMed/PubMed Central. These databases support the systematic search of many topics in health and healthcare. We screened all papers about the neurosyphilis in the primary/secondary health care setting under the search terms “pathogenesis of neurosyphilis,” “meningovascular syphilis,” “early secondary syphilis,“ “secondary syphilis,” We selected for review those that were relevant to these issues. For practice guidelines, we reviewed the references of each included manuscript. After this first process, we systematically searched the following electronic library databases)): Cochrane Library, Global Health, CINAHL, Web of Science (Clarivate Analytics), EMBASSY. The aim was to select the original research studies related to the abovementioned search strategy. After a confident peer-review process, the search was restricted to full-text Spanish, Portuguese, and English-language publications.
All studies were retrieved using MeSH, as before cited, and we only included aspects within the scope of the current work.
Inclusion and exclusion criteria
We selected randomized controlled trials or quasiexperimental studies published in peer-reviewed journals. The studies were excluded if they evaluated interventions for other types of secondary/tertiary syphilis. In addition, this review was also limited to studies involving adult patients and published in English, Spanish or Portuguese.
Study selection
We performed the literature search and scanned all articles by title and abstract. LdeFIV and HFS independently screened articles in full text for eligibility. It was followed by a discussion to establish a consensus on which studies were included, mainly when there was ambiguity.
Quality appraisal
Four areas of study quality were assessed: Selection bias, study design, health status, blinding process, reasons for dropout or withdrawal, and data collection methods. In addition, LdeFIV independently carried out a methodological quality assessment and then verified by HFS.
Data extraction
A data extraction mechanism was developed to extract research data about the setting, study design, demographic profile of patients, methods, measurement tools, and timing of assessments and outcomes. In addition, crucial information on the intervention for secondary data analysis studies was extracted from either the primary article or an earlier published manuscript. LdeFIV conducted the data extraction; consensus was achieved through discussion among LdeFIV/HFS.
Methods of analysis
Data syntheses were programmed to comprise the narrative analysis and intervention synthesis of selected manuscripts based on the PRISMA methodology.
Extracted data were initially synthesized using textual descriptions to determine the characteristics of the selected studies, and then they were grouped, clustered, and presented in tabular form.
Study and cohort selection
We select prospective and retrospective case reports, crosssectional studies, cohort studies, case-control studies, case series, reviews, controlled clinical trials, and meta-analyses releasing data on inclusion criteria.
Data collection process
The selected information is extracted from each manuscript with Microsoft Excel in a structured coding scheme. The data collected included pathogenesis of syphilis, clinical features, location of population size, gender and age distribution, and the investigations used to confirm the diagnosis when applicable. In cases where there was uncertainty regarding the interpretation of the selected data or how it could be used, we analyzed the situation until we arrived at an acceptable agreement.
Data synthesis
Our study used aggregate data when necessary, following the guidelines of PRISMA..
Quality assessment of selected publications
Initially, all studies were screened for bias using the Jadad scoring system as usual and included only those with Jadad scores ≥ 4 for further assessment [14].
Results
Study selection
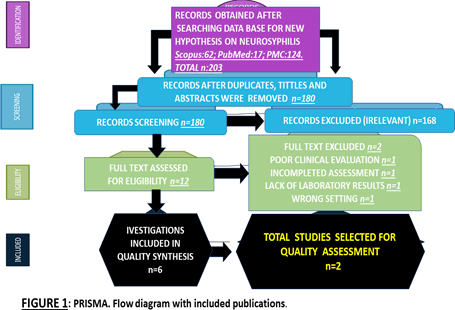
All selected manuscripts were peer-reviewed publications, and no one met all inclusion criteria. Below, A PRISMA flow chart for the literature searched is shown below (Figure 1).
Figure 1: Flow diagram of included manuscripts
Study characteristics
Ethics committees approved all publications included in this review, and patient consent was obtained; without this requirement, the pertained data were removed from this study.
Most studies (74.3%) were published in the last 5 years. Most investigations were conducted in the United States of America/Canada (49.1%), followed by the Asian continent (21.3%), the European continent (19.7%), and African countries (12%). The origin of 38% of cases was not identified. Most studies (79.9.7%) focused on people older than 18. The total of publications identified was n=203; after duplicate removal, n=180; after full text excluded, n=12; for quality synthesis, n=6; for quality assessment, n=2, which provides some new proposal for the pathogenesis of Ns [21,22]. In Sub Saharan Africa, only one publication was done.
Case report
An 18-year-old lady complained of a five-day history of inability to walk properly due to weakness in her lower limbs and lower back pain. She had no shortness of breath, headache, fever, cough, or difficulty talking. She denies any recent infection or trauma prior to the onset of her symptoms.
She had a previous hospitalization in July 2023, where she had urinary retention and fecal impaction, There is no one with similar symptoms at home. Both parents are alive, and her mother is hypertensive on treatment. No history of neurological condition in her family or other relevant information is reported. On examination: The patients look clinically well lying in bed, alert, and cooperative line inset. Pulse: 82 bpm, BP: 112/71 mm, Resp Rate: 18 rpm, Temp: 36.4°C. No jaundice, no pallor, no clubbing, no cyanosis, no oedema, no lymphadenopathy. Level of consciousness: GCS 15/15. Alert and well-orientated in time, place, person, and situation. Meningeal signs: No neck stiffness, negative Kerning’s, and negative Brudzinski’s signs. All cranial nerves examined were normal, and no focal neurological signs were found except 4/5 grade of power on lower limbs, with moderate spasticity, hyperreflexia ++, average muscle bulk and absent Babinsky sign. Other system examinations showed unremarkable findings.
Laboratory investigation: Cerebrospinal fluid analysis: Appearance: clear (N), CSF Glucose:3.2, CFS Protein: 0.65 (H), CFS adenosine deaminase: 0.1 (N). Cell count: Polymorphs: 0, Lymphocytes: 0 Erythrocytes: 0, Gram stain: No bacterial observed, Cryptococcal Latex Antigen Test: Negative, Treponema pallidum hemagglutination assay and rapid plasma reagin test were positive in serum and CSF samples. Fluorescent Treponemal Antibodies (FTA-Abs) were recorded as reactive.
Complete blood count: White cell count: 7.65 (N), hemoglobin: 13.8 (N), MCV: 94 (N), MCH: 30.6(N), Platelets: 315 (N), ESR: 53 (H) (suggestive of a recent inflammation), CRP: 7 (N). Sodium: 136 (N), Potassium: 3.9 (N), Chloride: 102 (N), CO2: 20 (N), Urea: 3.8 (N), Creatinine: 73 (N), eGFR: >60 (N). Liver function test: Total bilirubin: 7, Total Protein: 83, Albumin: 46, AST: 33, ALT: 62, ALP: 72, GGT: 33. Lipid Profile Cholesterol: 3.41 (N), TAG: 0.66 (N), LDL: 2.06 (N), HDL: 1.05 (N), Thyroid Function TSH: 3.02 (N), Free T-3: 6.8 (N), Free T-4: 118.1 (N).
In other Tests, Serum aquaporin-4 and myelin oligodendrocyte glycoprotein antibodies were negative, and Treponema pallidum Hemagglutination (TPHA) was positive. Serum angiotensin-converting enzyme, antinuclear antibody, ANCA, and viral markers for HIV, hepatitis B and C were negative. Vit B12: 378 (N), Folate: 45.3(N), INR: 1.12 (N), HIV Elisa: Negative, RPR: Positive, NCC Elisa: Negative, HSV: Positive, Tumor Market: All normal. Imaging: MRI of the spine, with contrast, confirmed a longitudinally extensive T2/FLAIR hyperintensity extending from the T4 to T9, involving more than two-thirds of the cross-sectional area with SC expansion. Post-contrast enhancement was seen in lower T6/T8 regions.
Treatment: Pharmacological: Supplants: To help minimize and prevent the progression of the disease, vitamin D 50 000 IU PO Weekly, thiamine 100 mlg PO daily 7/7 days, folate 5 mlg PO 7/7 days, pyridoxine 25 mlg PO 7/7 days, analgesic: For pain management panado1g PO 6 hourly 7/7 antibiotic therapy: Benzyl Penicillin 20 MU IV daily (in 4 doses-6 doses) 10/7 days, or Ceftriaxone 2 g IV daily 10-14/7. Non-Pharmacological: Physiotherapy and occupational therapy. In the ward, the patient is kept on supplements and analgesics for pain control. She is also receiving rehabilitation therapy from occupational therapists and physiotherapists. Long-term management of this patient will involve regular check-ups with the occupational therapist and physiotherapist after discharge until the function returns to normal.
Comments and concluding remarks
We identified 2 articles with similar cases reported in the medical literature but released no new hypotheses about the pathophysiology of Ns and only one related to epidemiology of Ns was published in our continent.
Brief comments on the case presentation
Our patient did not notice any round-painless sores at the external genitals of several weeks’ duration, and she denied any red-brown spots on the soles of the feet and the palms of the hands or skin or any skin rash during her previous 3 years of sex activities. Our patient developed symptomatic neurosyphilis before TP in the CSF was confirmed and never received antibiotic therapy before the current hospital admission. Our patient is HIV-negative, and the diagnosis of early Ns affecting the SC is based on her clinical symptomatology, clinical exam and examination of the blood and cerebrospinal fluid, such as serum tests for Sy using treponemal tests like Fluorescent Treponemal Antibody Absorption (FTA-ABS) or nontreponemal tests, such as Venereal Disease Research Laboratory test (VDRL) and Rapid Plasma Reagin (RPR) results. Our patient did not complaints about headache, nausea, cranial nerve neuropathies, vomiting, stiff neck, confusion, neurovascular complications like focal neurological signs due to ischemic stroke-like caused by infectious vasculitis, signs of posterior uveitis/panuveitis with decreased visual acuity, forgetfulness, personality changes, altered judgment, pupillarity abnormalities ataxia, or bowel and bladder dysfunction. Our case did not present grotesque skin lesions like nonpruritic erythematous rash, systemic symptoms, life-threatening complications, pharyngitis/ laryngitis, generalized lymphadenopathy, or any other clinical features described in cases with malignant Sy [15].
According to our personal experience, CSF abnormalities are related to the stage of the disease, and LP is strongly recommended in cases who present with ocular or neurologic disease that could be caused by Sy and in cases with HIV comorbidity Sy at any stage. CSF VDRL is particular; however, other authors reported that sensitivity ranges from only 30%-70% [2]. We prefer CSF VDRL over CSF RPR for diagnosing Ns and confirmed that the CSF treponemal antibody test is susceptible but not specific. Nonetheless, if the clinical suspicion for Ns is remarkably high, it could not be used to rule out Ns. We also hypothesized that CSF findings in cases with Ns should include high albumin levels and mild mononuclear pleocytosis. We treated our patient with a single dose of penicillin G benzathine, 2.4 million units intramuscularly, with excellent clinical response.
On the other hand, for cases presenting with late Sy, tertiary Sy or late latent Sy, administering 2.4 million units of IM penicillin G benzathine once weekly for 3 weeks is the best choice, which the Centers for Disease Control and Prevention in Atlanta, USA supports. As we represented in the table, the first regimen is 3 million to 4 million units of penicillin G IV every 4 hours for 10 days to 14 days, and the alternative scheme is 2.4 million units of IM procaine penicillin G daily plus 500 mg of probenecid orally 6 hourly for 10 days to 14 days, notwithstanding if the patient complaint mild penicillin allergy, re-challenging the case or desensitization is mandatory. Otherwise, IM/IV ceftriaxone can be used.
The meningovascular syphilitic Spinal Cord (SC) involvement in our patient was confirmed clinically and by investigations. SC’s involvement in Sy includes TD (prototypical presentation), meningovascular disease, and meningomyelitis. Less than 15 cases of meningomyelitis associated with Ns have been published in the literature. Agarwal et al. (2023) reported a case of Sy meningomyelitis presented with confirmed Longitudinally Extensive Transverse Myelitis (LETM) [16].
The correlation found between the type of Ns, clinical features, and laboratory results is summarized in Table 1, which shows data like those reported in the medical literature [2].
Brief comments on serologic and clinical features of early and late established neurosyphilis
Knowing that the TP invade the CNS after a few days from the primary infection, we hypothesized that the secretory/ excretory action of glutamate among other amino acids stimulates the polarization of innate glial cells into M1 with proinflammatory effect and M2 with anti-inflammatory activity, which explains all the clinical features or asymptomatic presentations and laboratory findings of Ns as early as 12 or 24 months after the primary infection while late forms like general paresis and TD respond to different pathophysiology.
Table 1 shows all stages of Ns according to clinical features and laboratory test findings. It has quite often seen presentations of early Ns characterized by asymptomatic meningitis with a cellular reaction in the CSF only, which headache, meningeal signs, cranial nerve palsies, and blindness or deafness have characterized. In a previous study of aseptic meningitis made on 60 patients from our country, 3.3% of cases were due to Sy [2].
Table 1: Types of Ns according to clinical manifestations and laboratory findings
| Stage of ns | Types | Clinical manifestations | Laboratory findings |
|---|---|---|---|
| Early stage | Asymptomatic | Free of symptoms and signs and pleocytosis after few weeks | Reactive VDRL serology and CSF-VDRL* |
| Early stage | Syphilitic meningitis | Meningeal signs, headache, craneal nerves involvement(cni), altered level of conciouness (alc), delirum after weeks or months. | Reactive reactive vdrl serology and CSF VDRL, CSF FTA-ABS and pleocytosis-10-450/mm3* |
| Early or late stage | Meningovascular syphillis | Menigeal syndrome, stroke, cni, progressive myelopathy (meningomyelitis) with Sphincter Dysturbance (SD) | Reactive VDRL serology and CSF VDRL, leucocytosis (5-120 mm3) |
| Late stage | General paresis | Neuropsychiattric manifestations,progressive cognitive decline, personality changes, argyll-robertson pupils (50%), dysarthria, tremors, manic delusions | Reactive VDRL serology (50%) and CSF VDRL, reactive CSF FTA-ABS and pleocytosis, Permanent Mild Pleocytosis (PMCP)
|
| Tabes dorsallis | Remarkable romberg’s text, ataxic gait, argyll-robertson pupil (>75%), loss of deep touch and propioception, paraparesis with areflexia, SD, charcot arthropathy | Probably non-reactive VDRL serology but reactive CSF VDRL, reactive CSF FTA-ABS and PMCP |
MV Sy is a well-recognized form of meningitis with vasculitis (small and medium-size arteries) in the CNS, leading to ischemic strokes and a wide variety of spinal cord disorders, which are usually interposed temporally between 2 forms of Ns presentation like nearly and later forms of Ns almost always seen between 1 year to 10 years after the primary infection. After the confirmation that GP is due to anatomical damage of the brain, the concept of madness was removed from the vocabulary of the medical community. It incorporated the terminology of mental disorders due to structural brain injury, which the most common presentation is frontotemporal dementia with prominent clinical manifestations such as grandiose delusions like an African emperor, owner of the entire world, transformer of iron in gold using a repetitive speech pattern, seizure disorders, depression, psychosis, personality changes, new types of progressive cognitive decline.
Nevertheless, TD is typically characterized by ataxic gait (“stamp and stick” sound), vestibular signs, Argyll Roberton pupil, Charcot joints (neuropathic arthropathy), alarming lancinating pains in the abdomen simulating acute abdomen and severe pain on the limbs resembling peripheral vascular thrombosis. Fortunately, TD is much less frequent than GP for unknown reasons [2].
Brief comment on the laboratory investigations
The laboratory tests for confirmation of Ns are based on the elevations of the CSF white cell count and albumin level plus reactive serum serology test. CSF serologic and blood tests for Ns are classified as nontreponemal tests using Venereal Disease Research Laboratory (VDRL) or Rapid Plasma Reagin (RPR) techniques or treponemal tests using Fluorescent Treponemal-Antibody Absorption (FTA-ABS) shown in Table 2.
Table 2: Laboratory test For Ns
| Test | Sensitivity | Sensitivity | Specificity |
|---|---|---|---|
| Early Ns (percent) | Late, symptomatic Ns (percent) | Late, symptomatic Ns (percent) | |
| Serology test | - | - | - |
| Serum VDRL/RPR | 100 | 50-80 | 92 |
| CSF VDRL | 78 | 35-75 | 100 |
| CSF FTA-ABS, TPHA | 100 | ÃÂ?± 97 | ÃÂ?± 65 |
| CSF content | - | - | - |
| WCC>5-10mm3 | 100 | 96 | ÃÂ?± 98 |
| Protein>0.45 | 92 | 94 | <50 |
The graphical correlation between the clinical features of syphilitic patients and the positivity of serological test results is shown in Figure 2, and its presentation is selfexplanatory.
Brief comments on sensitivity and specificity of laboratory tests for neurosyphilis
Serum nontreponemal studies are reactive in most patients presenting Ns (during and after the secondary stage), but it can become nonreactive in late Ns because of waning titters over time, mainly after medical therapy. The CSF VDRL test is more specific for Ns if the sample is not contaminated with blood but is only 35% to 75% sensitive, and the false negative rate for the CSF RPR test might be higher [2]. In cases where the CSF VDRL test is negative in a symptomatic patient that is consistent with Ns, CSF treponemal tests are strongly recommended. The sensitivity/specificity of serologic laboratory tests for Ns and other investigations are shown in the above table.
Figure 2: Graphical correlation between clinical features of syphilis and serology findings. Shows the curve for the cerebrospinal fluid Fluorescent Treponemal-Antibody Absorption (FTA-ABS) test and the uncertain test results in late Ns. The percentage of patients whose serum non-treponemal test results stay reactive is lower if the patients have been treated for Sy (and would not be likely to acquire Ns) than if the patients are untreated. In the lower panel, the prevalence of each form of neurosyphilis is represented. RPR denotes rapid plasma reagin, and VDRL
In untreated patients, serum, and CSF treponemal tests are usually positive for the lifetime, but the CSF test may become negative years after medial therapy of uncomplicated Sy in up to 15% of cases. In contrast, a false positive result of a CSF FTA-ABS test caused by blood contamination can happen if the number of red cells is more than 1000 per mm3. Pragmatically, a diagnosis of symptomatic Ns is unlikely unless a serum FTA-ABS investigation is reactive (reflecting previous Sy) and a CSF VDRL test is reactive (indicating Ns). Notwithstanding, to rule out asymptomatic Ns, a nonreactive CSF treponemal test is enough but not specific enough. As we proved in our case presenting neurological manifestations, if the serological test confirms the presence of Sy, the examination of the CSF is mandatory, and the following of the level of CSF white cells to determine the efficacy of the medical therapy is also recommended. Based on the previous postulate, we suggest that another course of antibiotics should be implemented if the pleocytosis in the CSF persists beyond 6 months, if it is still present after 2 years of therapy, or if the RPR titter does not decrease. In our setting, where the prevalence of HIV/AIDS is remarkably high, the presence of prolonged CSF pleocytosis should be considered with caution, and the previous recommendation is not certain.
The estimates calculations of serologic sensitivity/ specificity are strongly related to the choice of controls, the current stage of Sy, and the accuracy confidence of laboratory/clinical features used as a reference. Xie and colleagues, studying the actual value of nontreponemal tests, found a higher pooled specificity and concluded that treponemal tests have a higher pooled sensitivity in diagnosing Ns on CSF and proposed it as an investigation of choice [17].
Over decades, CSF pleocytosis decreases gradually and is accompanied by a mild increase in albumin level, as is shown in the figure.
Brief comments on the updated treatment of neurosyphilis
As a general agreement, the progressive diminishing rates of GP from the past 50 years is a clear indication of the role played by parenteral penicillin therapy for early Sy and the subsequent prevention of Ns despite the differences in the therapy guidelines from Europe, the United Kingdom and the United States of America as we summarized in Table 3 [2].
Table 3: Therapy guidelines from Europe, the United Kingdom and the United States of America
| Country | Recommended therapy for early and late Ns |
|---|---|
| Europe | IV benzylpenicillin, 3 million-4 million units 4 hourly for 10 days-14 days or IV ceftriaxone, 1 g-2 g daily for 10 days-14 days, or penicillin G procaine, 1.2 million-2.4 million units IM daily plus probenecid, 500 mg PO 6 hourly for 2 weeks |
| United Kingdom | Penicillin G procaine, 1.8 million-2.4 million units IM daily plus probenecid, 500 mg PO 4 times a day or benzylpenicillin, 1.8-2.4 IV 6 times a day for 2 weeks and prednisolone, 40 mg-60 mg daily for 72 hours, starting 24 h before the first penicillin dose |
| USA (CDC, Atlanta) | Aqueous crystalline penicillin G, 3 million-4 million units IV every 4 h or 18 million-24 million units every day as a continuous infusion, for 10 days-14 days; or if adherence is ensured, penicillin G procaine, 2.4 million units IM every 24 h, plus probenecid, 500 mg PO 6 hourly for 10 days-14 days |
Based on the reported data about the outcome of patients with Ns under penicillin therapy, we hypothesized that therapy with antibiotics probably does not improve the clinical features of Ns but frequently halts their progression. Even though penicillin is the medication of choice in cases where it is not recommended for whatever reason, tetracycline, ceftriaxone, or doxycycline can be effective.
Brief comments about the new hypotheses on the pathogenesis of neurosyphilis
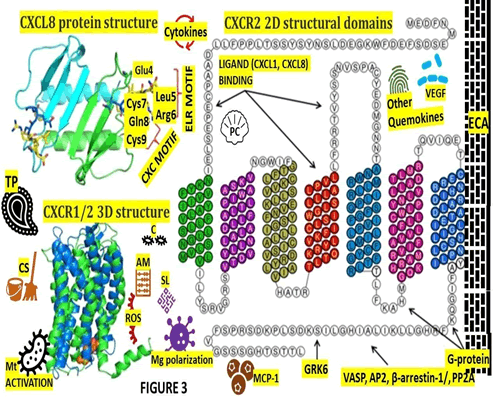
As we considered before, the CXCL8 Expression/Secretion (ES) may play a crucial role in the pathogenesis of Ns because It is well known that epithelial/endothelial cells, fibroblast, alveolar macrophage, and inclusive blood monocytes can secrete CXCL8 [18]. Some cells are affected by TP invasion, causing a cascade of responses to that insult. Several elements such as hypoxia, oxidative stress/Reactive Oxygen Species (ROS), cytokines (TNFα, INF β, interleukin-1, and interleukin-6), CXCL12, bacterial particles and other environmental stresses, and mediated by transcription factors, NF-κB and Activator Protein-1 (AP-1) can activate CXCL8 [19]. The pathogenesis of SC involvement in our case was commented on before, but we would like to highlight that our patient did not present an associated spine bone damage, which, although rare, can be seen in cases with tertiary Sy [20].
Chemokine Ligand 13 (CXCL13) plays a relevant role in the recruitment of B lymphocytes in the CNS during NI caused by TP. Based on previous studies, we hypothesized that CXCL13 and Ns are closely interrelated and serve as significant biomarkers to determine the presence of NS from non-Ns/Sy in HIV patients [21].
Based on the article published by Waugh et al. (2023), we hypothesize on the role played by PCD/RCD (MLKL, TRADD, STUB1, DR5, IRF1) in the pathogenesis of NS [22]. The role played by OS (ROS), microglia polarization, Toll-Like Receptor (TLR) signaling, regulated necroptosis, apoptosis, pyroptosis, PANoptosis, ferroptosis and Cuproferropanoptosis in the chronic infectious processes has been reported several times [23-29] recently and hypothesized that that mechanism might be included in the pathogenesis of Ns as are graphically represented in Figure 3. Figure partially adapted from Helen Ha et al. (2017) [19].
We also graphically represented the participation of some proposed elements such as mitochondria activation, IL- 6, IL-8, IL-17, INF-β, (VEGF), decreased secretion of (MCP-1), chemokines in the pathogenesis of Ns from the passage of TP across the vascular endothelial layer of the BBB secreting (ECM) components with increasing tight junction proteins/pericytes (Rouget cells) expression, OLG/OPC activity, and the cleaning system involved in chronic infectious diseases of the CNS.
Figure 3: Structure of CXCL8 and its receptors CXCR1/2. A. CXCL8 protein structure: The dimer structure was generated from the Protein Data Bank code PDB ID 1ICW. B. CXCR2 2D structural domains: The N-terminus (extracellular face) of CXCR2 is critical for ligand binding and specificity. Transmembrane domain 4 and extracellular loop 2 is also important for ligand binding. The G-protein couples to the C-terminus (cytoplasmic face) of CXCR2 and involves intracellular loop 3. Several proteins, such as G Protein Coupled Receptor Kinase 6 (GRK6), Vasodilator-Stimulated Phosphoprotein (VASP), β-arrestin1/2, Adaptor Protein-2 (AP-2), Protein Phosphatase 2A (PP2A) also associate with the C-terminus of CXCR2 to mediate different signaling cascades. C. CXCR1/2 3D structure: CXCR1 solid state NMR structure (PDB: 2LNL, green) aligned with CXCR2 homology model (blue). The predicted binding mode of the CXCR2 antagonist SCH527123 in the allosteric site located inside the CXCR2 receptor. Abbreviations: AM-adhesion molecule (ICAM-I;VE-cadherin ; F-actin ; E-selectin ; MCP-1) C-cytokines (IL-1β,TNF-a, IL-6, IL-8, IL-10, TGF-β), ECA: Endothelial cell activation; SL-serum lipoprotein (ApoA-I, apoB; HDL-C; TGs.); TP-Treponema pallidum; PC-Pericyte; Mg-Microglia, MCP1-Monocyte Chemoattractant Protein-1; ECM-extracellular Matrix; ROS-Reactive Oxygen Species, OLG/OPC-Oligodendrocyte/Oligodendrocyte Precursor Cell, VEGF-Vascular Endothelial Growth Factor; Mt-Mitochondria; CS-Cleaning System (MLV, GS, AQP4, CA). CXCL8 is a 72-amino acid peptide that has 3 antiparallel β-strands and one a-helix made up of C-terminal residues 57-72. The structure is stabilized by 2 disulfide bonds (Cys7-Cys34 and Cys9-Cys50) and the 2 cysteine residues (Cys7 and Cys9) are separated by one residue (Gln8), hence CXCL8 is classified as CXC chemokine. The CXCL8 exists as a dimer stabilized by hydrogen bonds between the first β-strand. Interactions between CXCL8 and CXCR1 N-terminal site-1 and play an important role for higher affinity of the receptor towards CXCL8 monomer than dimer
Conclusion
We hypothesized in Ns that the EC induce a signaling pathway able to modify the cytoskeleton and endothelial junctions at the BBB, allowing the extravasation of harmful material, which must be removed to the cervical lymphatic chain through the cleaning system composed by the Meningeal Lymphatic System (MLV), Glymphatic System (GS), Aquaporin 4 (QP4) and Corpus Amylacea (CA) as we reported for similar situations recently plus an increase expression of almost all before cited elements at the same time.
As far as we know, this is the first article proposing a new hypothesis on the pathogenesis of Ns based on the role played by OS (ROS), cytokines, chemokines, Mt activation, Mg polarization and many other mentioned proteins and enzymes.
Declarations
Consent for Publication
We obtained written informed consent for publication from our patient, including laboratory results. All information is fully available for any interested reader by request.
Manuscript writing process
HFS and LFIV. All authors have approved this version for publication.
Declaration of anonymity
All authors certified that they did not mention the names, initials, and other identity issues of this patient. Therefore, a complete anonymity is guaranteed.
Availability of data and material
All data supporting this report are available on reasonable request from the corresponding author.
Ethical Approval
The WSU/NMAH Ethical Committee did not request an additional ethical approval for this study.
Acknowledgement
We thank Prof Thozama Dubula, The Dean of Faculty of Health Sciences and Dr Kulile Moeketsi for their permanent support.
Competing Interest
Both authors declared that they performed this study without any commercial, financial, or otherwise relationships able to construe a potential conflict of interest.
Funding
Both authors declared that they did not receive financial aid or collaboration that could have influenced the results reported in this paper.
Authors’ Contributions
Study concept and design: HFS, and LFIV. Data collection from searched literature: HFS, and LdeFIV. Analysis of the obtained data was done by LdeFIV/HFS plus the first and final draft of this paper. The manuscript was revised by HFS and LFIV and it was supervised by HFS.
References
- B. Xie, T. Zhao, S. Zhao, J. Zhou, F. Zhao, Possible effects of Treponema pallidum infection on human vascular endothelial cells, J Clin Lab Anal, 36(2022):e24318.
- A.H. Ropper, Neurosyphilis, N Engl J Med, 381(2019):1358-1363.
- S.R.S. Mok, V. Punjabi, D.L. Shklar, Neurosyphillis presenting with normal pressure hydrocephalus in a 76-year-old man, Am J Case Rep, 13(2012):173-176.
- C.M. Marra, C.L. Maxwell, L.C. Tantalo, S.K. Sahi, S.A. Lukehart, Normalization of serum rapid plasma reagin titer predicts normalization of cerebrospinal fluid and clinical abnormalities after treatment of neurosyphilis, Clin Infect Dis, 47(2008):893â??99.
- W. Tang, S. Huang, L. Chen, L. Yang, J.D. Tucker, et al. Late neurosyphilis and tertiary syphilis in Guangdong Province, China: Results from a cross-sectional study, Sci Rep, 7(2017):45339.
- L. Jankowska, Z. Adamski, A. Polanska, M. Bowszyc-Dmochowska, K. Plagens-Rotman, et al. Challenges in the diagnosis of tertiary syphilis: Case report with literature review, Int J Environ Res Public Health, 19(2022):16992.
- C. Rich, D. Papanagnou, D. Curley, X.C. Zhang, Neurosyphilis: A simulation case for emergency medicine residents, Cureus, 10(2018):e2984.
- C.M. Marra, Neurosyphilis, Continuum, 21(2015):1714-28.
- M.R. Golden, C.M. Marra, K.K. Holmes, Update on syphilis: Resurgence of an old problem, JAMA, 290(2003):1510-4.
- M.L. Henninger, S.I. Bean, J.S. Lin, Screening for syphilis infection in nonpregnant adults and adolescents, JAMA, 328(2022):1243-1249.
- J. Fang, E. Partridge, G.M. Bautista, D. Sankaran, Congenital syphilis epidemiology, prevention, and management in the United States: A 2022 update, Cureus, 14(2022):e33009.
- T. Roy, A.D. Gupta, A.R. Islam, Optic neuritis presented as the only manifestation of neurosyphilis, Oman J Ophthalmol, 21(2023):161-164.
- J.J.B. Garcia, J.L. Coralde, M.A.C. Bagnas, K.J.O. Khu, Isolated cranial nerve VI palsy and neurosyphilis: A case report and review of related literature, IDCases, 27(2022):e01377.
- A.R. Jadad, R.A. Moore, D. Carroll, C. Jenkinson, D.J. Reynolds, Assessing the quality of reports of randomized clinical trials: Is blinding necessary, Control Clin Trials, 17(1996):1-12.
- J. Dimnik, M. Benko, V. Hosta, A. Murnik Rauh, A. Pagon, et al. Malignant syphilis in a female patient: A case report and mini-review, Trop Med Infect Dis, 7(2022):47.
- A. Agarwal, S. Joy, D. Garg, A. Garg, A.K. Srivastava, Neurosyphilis manifesting as longitudinally extensive transverse myelitis, Ann Indian Acad Neurol, 26(2023):587-589.
- J.W. Xie, M. Wang, Y.W. Zheng, Y. Lin, Y. He, et al. Performance of the nontreponemal tests and treponemal tests on cerebrospinal fluid for the diagnosis of neurosyphilis: A meta-analysis, Front Public Health, 11(2023):1105847.
- J. Wanninger, M. Neumeier, J. Weigert, S. Bauer, T.S. Weiss, et al. Adiponectin-stimulated CXCL8 release in primary human hepatocytes is regulated by ERK1/ERK2, p38 MAPK, NF-kappaB, and STAT3 signaling pathways, Am J Physiol Gastrointest Liver Physiol, 297(2009):G611-8.
- H. Ha, B. Debnath, N. Neamati, Role of the CXCL8-CXCR1/2 axis in cancer and inflammatory diseases, Theranostics, 7(2017):1543-1588.
- Y. Bai, F. Niu, L. Liu, H. Sha, Y. Wang, et al. Tertiary syphilis in the lumbar spine: A case report, BMC Infect Dis, 17(2017):513.
- Y.L. Zeng, Y.Q. Lin, N.N. Zhang, C.N. Zou, H.L. Zhang, et al. CXCL13 chemokine as a promising biomarker to diagnose neurosyphilis in HIV-negative patients, Springerplus, 5(2016):743.
- S. Waugh, A. Ranasinghe, A. Gomez, S. Houston, K.V. Lithgow, et al. Syphilis and the host: Multi-omic analysis of host cellular responses to treponema pallidum provides novel insight into syphilis pathogenesis, Front Microbiol, 19(2023):1254342.
- H.F. Sibat, L.F. Valdes, Meningeal lymphatic vessels and glymphatic system in neurocysticercosis, Clin Schizophr Relat Psychoses, 17(2023).
- H.F. Sibat, L.F.I. Valdes, Novel hypotheses on the role of oligodendrocytes in neurocysticercosis: Comprehensive review, Clin Schizophr Relat Psychoses, 17(2023).
- H.F. Sibat, L.F.I. Valdes, The role of pericytes in neurocysticercosis: Comprehensive review and novel hypotheses, Clin Schizophr Relat Psychoses, 2013.
- H.F. Sibat, L.F. Valdes, Novel hypotheses on the role of microglia and panoptosis in neurocysticercosis, Clin Schizophr Relat Psychoses, 17(2023).
[Crossref]
- A.H. Del Rio-Romero, H.F. Sibat, L.F. Valdes, E. Vega-Novoa, The role of oxidative stress in neurocysticercosis: A comprehensive research, Clin Schizophr Relat Psychoses, 17(2023).
- H. Foyaca-Sibat, A.H. Del Rio-Romero, E. Vega, L.F. Valdes, The role of ferroPANoptosis in neurocysticercosis: A comprehensive review, Interdiscip Perspect Infect Dis, 2023.
- H. Foyaca-Sibat, A.H. Del Rio-Romero, E. Vega, L.F. Valdes, Our hypotheses about the role of cuproferropanoptososis in neurocysticercosis and a comprehensive review, J Drug Alc Res, 12(2023):1-9.
[Crossref]
Copyright: © 2024 Lourdes de Fatima Ibanez Valdes, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.